New research provides important insights into the role played by the immune system in preventing—and in some cases increasing the severity of—COVID-19 symptoms in patients. It also finds clues to why some people experience “long COVID.”
Among the key findings, which have not yet been peer-reviewed, are:
- Individuals who have asymptomatic or mild disease show a robust immune response early on during infection.
- Patients requiring admission to hospital have impaired immune responses and systemic inflammation (that is, chronic inflammation that may affect several organs) from the time of symptom onset.
- Persistent abnormalities in immune cells and a change in the body’s inflammatory response may contribute to ‘long COVID.”
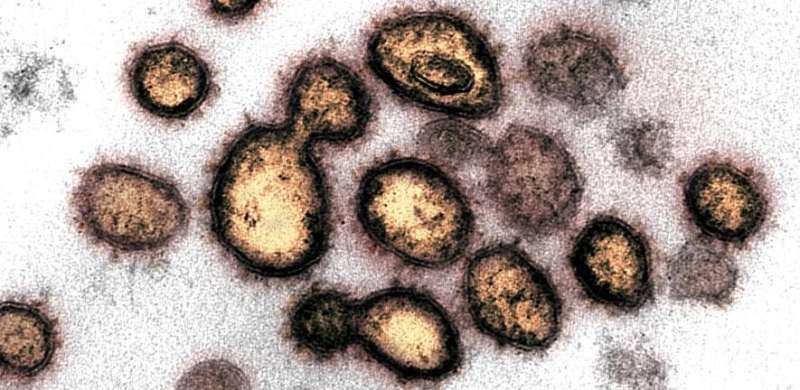
The immune response associated with COVID-19 is complex. Most people who get infected by SARS-CoV-2 mount a successful antiviral response, resulting in few if any symptoms. In a minority of patients, however, there is evidence that the immune system over-reacts, leading to a flood of immune cells (a ‘cytokine storm’) and to chronic inflammation and damage to multiple organs, often resulting in death.
To better understand the relationship between the immune response and COVID-19 symptoms, scientists at the University of Cambridge and Addenbrooke’s Hospital, Cambridge University Hospitals NHS Foundation Trust, have been recruiting individuals who test positive for SARS-CoV-2 to the COVID-19 cohort of the NIHR BioResource. These individuals range from asymptomatic healthcare workers in whom the virus was detected on routine screening, through to patients requiring assisted ventilation. The team take blood samples from patients over several months, as well as continuing to measure their symptoms.
In research published today, the team analyzed samples from 207 COVID-19 patients with a range of disease severities taken at regular interviews over three months following the onset of symptoms. They compared the samples against those taken from 45 healthy controls.
Because of the urgent need to share information relating to the pandemic, the researchers have published their report on MedRXiv. It has not yet been peer-reviewed.
Professor Ken Smith, senior co-author and Director of the Cambridge Institute of Therapeutic Immunology & Infectious Disease (CITIID), said: “The NIHR BioResource has allowed us to address two important questions regarding SARS-CoV-2. Firstly, how does the very early immune response in patients who recovered from disease with few or no symptoms, compare with those who experienced severe disease? And secondly, for those patients who experience severe disease, how rapidly does their immune system recover and how might this relate to ‘long COVID’?”
The team found evidence of an early, robust adaptive immune response in those infected individuals whose disease was asymptomatic or mildly symptomatic. An adaptive immune response is where the immune system identifies an infection and then produces T cells, B cells and antibodies specific to the virus to fight back. These individuals produced the immune components in larger numbers than patients with more severe COVID-19 managed, and within the first week of infection—after which these numbers rapidly returned to normal. There was no evidence in these individuals of systemic inflammation that can lead to damage in multiple organs.
In patients requiring admission to hospital, the early adaptive immune response was delayed, and profound abnormalities in a number of white cell subsets were present. Also present in the first blood sample taken from these patients was evidence of increased inflammation, something not seen in those with asymptomatic or mild disease. This suggests that an abnormal inflammatory component to the immune response is present even around the time of diagnosis in individuals who progress to severe disease.
The team found that key molecular signatures produced in response to inflammation were present in patients admitted to hospital. They say that these signatures could potentially be used to predict the severity of a patient’s disease, as well as correlating with their risk of COVID-19 associated death.
Dr. Paul Lyons, senior co-author, also from CITIID, said: “Our evidence suggests that the journey to severe COVID-19 may be established immediately after infection, or at the latest around the time that they begin to show symptoms. This finding could have major implications as to how the disease needs to be managed, as it suggests we need to begin treatment to stop the immune system causing damage very early on, and perhaps even pre-emptively in high risk groups screened and diagnosed before symptoms develop.”
The researchers found no evidence of a relationship between viral load and progression to inflammatory disease. However, once inflammatory disease was established, viral load was associated with subsequent outcome.
The study also provides clues to the biology underlying cases of ‘long COVID’ – where patients report experiencing symptoms of the disease, including fatigue, for several months after infection, even when they no longer test positive for SARS-CoV-2.
The team found that profound alterations in many immune cell types often persisted for weeks or even months after SARS-CoV-2 infection, and these problems resolved themselves very differently depending on the type of immune cell. Some recover as systemic inflammation itself resolves, while others recover even in the face of persistent systemic inflammation. However, some cell populations remain markedly abnormal, or show only limited recovery, even after systemic inflammation has resolved and patients have been discharged from hospital.
Dr. Laura Bergamaschi, the study’s first author, said: “It’s these populations of immune cells that still show abnormalities even when everything else seems to have resolved itself that might be of importance in long COVID. For some cell types, it may be that they are just slow to regenerate, but for others, including some types of T and B cells, it appears something is continuing to drive their activity. The more we understand about this, the more likely we will be able to better treat patients whose lives continue to be blighted by the after-effects of COVID-19.”
Professor John Bradley, Chief Investigator of the NIHR BioResource, said: “The NIHR BioResource is a unique resource made possible by the strong links that exist in the UK between doctors and scientists in the NHS and at our universities. It’s because of collaborations such as this that we have learnt so much in such a short time about SARS-CoV-2.”
Craig Brierley, University of Cambridge

