A new UC San Francisco study has shown that a cancer-killing (“oncolytic”) virus currently in clinical trials may function as a cancer vaccine-in addition to killing some cancer cells directly, the virus alerts the immune system to the presence of a tumor, triggering a powerful, widespread immune response that kills cancer cells far outside the virus-infected region.
Using novel approaches to examine exactly how oncolytic viruses attack tumors, issue of Cancer Research provided surprising insights about how a viral infection can cooperate with the immune system to attack cancer cells. The study highlights an opportunity to combine this form of therapy with cancer immunotherapy drugs such as checkpoint inhibitors, which unleash the immune system’s full cancer-fighting power.
The idea that viruses could fight cancer goes back to the early 20th century, when doctors noted that cancer patients sometimes experienced dramatic remission after getting viral infections. Researchers have been developing oncolytic viruses since the 1980s, but following the U.S. Food and Drug Administration’s 2015 approval of Amgen’s Imlygic (T-Vec) as the first oncolytic viral therapy in the U.S., such viruses have become a closely watched area of therapeutic development.
Viruses appear capable of attacking tumors in a number of different ways by directly infecting them, by releasing tumor proteins that trigger a broad immune response against the cancer, and by damaging the blood supply tumors need to survive. To better understand the underlying mechanisms of these viral therapies, a collaboration was forged between UCSF vascular researcher Donald McDonald, MD, Ph.D., and researchers at San Francisco-based biotech SillaJen Biotherapeutics Inc. (formerly Jennerex Biotherapeutics, Inc.)
SillaJen is developing an oncolytic viral therapy called Pexa-Vec, currently in phase III and phase Ib/II clinical trials for use against primary liver and colorectal cancers, respectively. Pexa-Vec is an engineered virus based on the harmless vaccinia cowpox virus, also the basis for the original smallpox vaccine. Early observations suggesting that the virus might attack cancer in part by damaging blood vessels that feed tumor growth.
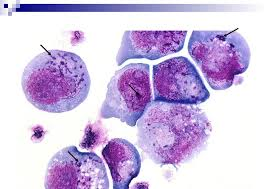
To study how the modified virus attacks tumors, researchers in the McDonald lab injected it intravenously into mice genetically modified to develop neuroendocrine pancreatic cancer. They found that the virus failed to infect healthy organs or make the animals ill, but succeeded in infecting blood vessels within tumors. These initial infections caused the vessels to leak and expose the tumor cells to the virus. In these experiments, the virus managed to infect and destroy only a small proportion of tumor cells directly, the researchers found, but within five days of the initial infection, the rest of the tumor began to be killed by a powerful immune reaction.
At first small spots of the tumor were infected, but then most of the tumor started to die. The researchers found that by killing some tumor cells directly, the viral infection exposed tumor proteins that could be detected by the immune system, triggering an immune attack on the rest of the tumor. The researchers demonstrated this by temporarily getting rid of the immune system’s cancer-killing cells, called CD8+ or cytotoxic T cells, and showing that without these cells, the virus killed only the initial five percent of cancer cells.
When the researchers examined the tumors, they discovered that the second drug acted by making the immune system hyper-alert to tumor proteins released by the viral infection, rather than through effects on tumor blood vessels. This finding suggests that pairing Pexa-Vec’s ability to awaken the immune system to previously ignored signs of cancer with the newest generation of checkpoint inhibitors, which act by unleashing the immune system’s full force, might be an extremely potent combination therapy.
haleplushearty.blogspot.com