Just one night of disturbed sleep means you are less capable to control posture and balance the day after a single bad night sleep decreases your chance of controlling posture according to researchers at the University of Warwick, who have used state of the art sensors to monitor sleep and balance implications could be that older people who have had a bad night sleep are the most at risk of a fall.
Innovative solutions of how to prevent imminent falls can now be researched Disturbances during sleep decreases capability to control posture and balance according to researchers from the Department of Engineering and Warwick Medical School at the University of Warwick who have an article published today in Scientific Reports.
This is the first study demonstrating the relationship between disrupted sleep and the reduced capability to control posture and balance, and it could pave the way to new interventions to prevent falls in later life, should the results be confirmed by other studies on older adults.
The research shows that fragmented and disrupted sleep leads to acute balance deficit.
The study was conducted by the School of Engineering in collaboration with Warwick Medical School at the University of Warwick.
A sample of healthy adults underwent sleep and balance assessment over two consecutive days, in order to determine the links between day-to-day variations in sleep quality and balance.
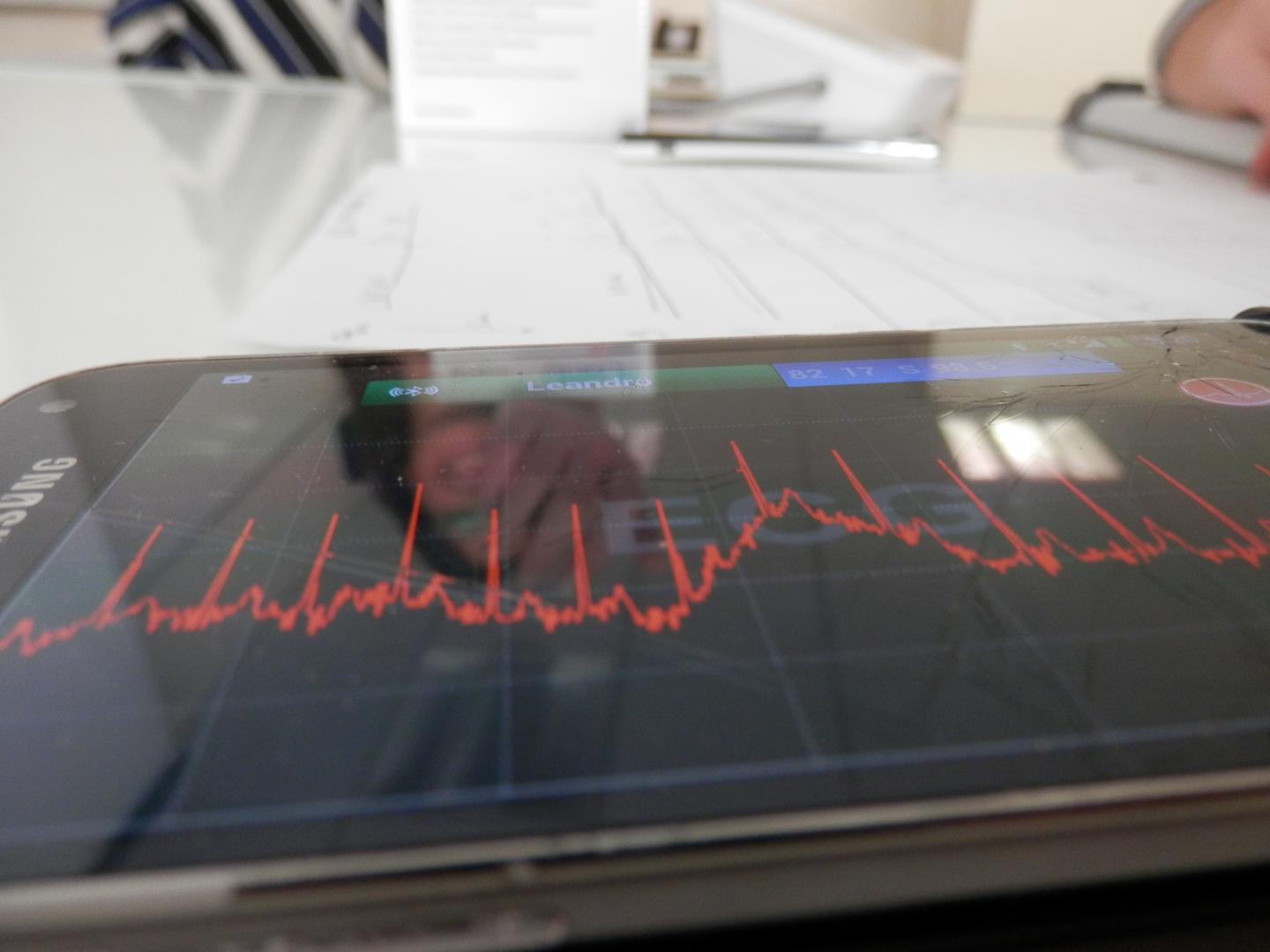
State-of-the-art wearable sensors were used for in-home sleep monitoring and balance testing. These findings are relevant to pave the way to the design of fall prevention programs in populations and settings where normal sleep is frequently disrupted, such as older people and hospital wards.
Dr Leandro Pecchia, team leader of the research from the School of Engineering at the University of Warwick says:
“We all have direct experience of this. When we do not sleep well, we may feel a little dizzy and our capability to control our posture and balance is somehow diminished. When we are fit and in good health, our body is able to adapt and we develop a strategy to keep our balance, avoiding falls and incidents. This ability is reduced with ageing or when there are other concomitant conditions that may compromise our ability to adapt.”
Prof Francesco Cappuccio, Head of the Sleep, Health & Society programme at the University of Warwick’s medical school, explains:
“The results obtained in healthy normal volunteers are surprising, given the ability at younger ages to compensate for such acute and short-lived sleep disruptions. We would expect more dramatic effects when these experiments be replicated in older people, whose vulnerability to sleep disruption, postural hypotension and risk of falls is much greater”.
Dr Lenadro Pecchia continues:
“These results could contribute to the understanding of in-hospital falls. Hospitalised older patients find themselves in a frail condition, sleeping in an unfamiliar environment, with unusual nocturnal light and noises from other patients and nurses, and perhaps being administered more than one drug. Waking-up to go to the toilet can be more challenging than we can imagine. Having a nurse for each bed is not practical in the modern NHS and not well accepted by many older people. We need to learn how to use available technology to detect early the changes in sleep so that we can design personalised interventions that may avoid falls in the next day. One of the problems in fall prevention is that we know a frail subject will fall, but it is very difficult to predict when. Our study is first step towards finding a solution.”

