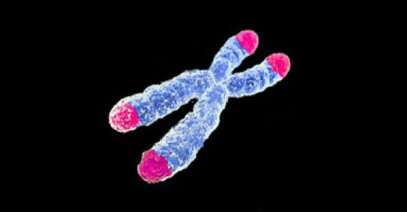
Healthy cells have a built-in self-destruct mechanism: Strands of DNA called “telomeres” act as protective caps on the ends of your chromosomes. Each time a cell replicates, telomeres get a little shorter. Think of it like filing your nails with an Emory board—after enough filing, you hit your fingertip—ouch! In the case of healthy cells, after enough replications, telomeres are “filed” away, leaving bare ends of the chromosomes exposed. At that point, healthy cells are inactivated or die. The eventual loss of telomeres is a major reason you are not immortal. This cellular mortality is also a major way your body fights cancer.
That’s because a hallmark of cancer is cellular immortality. And for that to happen, somehow, some way, cancer cells have to break the body’s system of telomere degradation—cancer needs to keep chromosomes safely capped. One way they do it is by spackling new DNA onto telomeres faster than it’s lost. This involves supercharging the gene that codes for new telomere material.
The TERT gene is the third most commonly mutated gene in cancer. When cancer over-activates TERT, it manufactures more of the enzyme “telomerase,” which rebuilds telomeres faster than they are degraded. With telomeres being built faster than they degrade, cancer cells gain immortality. Especially cancer like melanoma, glioblastoma, and bladder cancers (among others) are defined by TERT mutation. It’s likely that without TERT mutation, there would be none of these cancers.
Unfortunately, despite a massive effort by research and pharmaceutical communities, there is no silver bullet that successfully turns off over-activated TERT in human cancer patients (though anti-TERT drugs have done well against cancer cells in dishes and even in mouse models).
Now a study by Nobel Laureate, Thomas Cech, Ph.D., University of Colorado Cancer Center investigator and Director of the Biofrontiers Institute at University of Colorado Boulder, offers an intriguing new way to target TERT over-activation. Between a gene and its expression is an important step: The blueprints from the TERT gene have to get from the cell’s nucleus out into the cell’s cytoplasm, where tiny manufacturing centers called ribosomes make these TERT blueprints into the telomerase enzyme that rebuilds telomeres. (That’s a difficult sentence—consider rereading before continuing…)
The current study, published in the Proceedings of the National Academy of Sciences, shows that unlike “messenger RNA” (mRNA) for other genes, the messengers in charge of bringing TERT blueprints to ribosome manufacturing centers dally in the cell nucleus.
Let’s let Dr. Cech deliver the punchline:
“Our hypothesis is that there’s a special mechanism for transporting TERT mRNA into the cytoplasm that is really slow or inefficient, and that this is another level of regulation that most genes don’t need. But TERT needs this special step in regulating the transport of mRNA—and if that’s the case, maybe that could be a new target for interfering with this transport step. Maybe we could attack TERT in cancer cells by keeping mRNA trapped in the nucleus,” Cech says.
In other words, maybe the silver bullet in the fight against TERT over-activation has nothing to do with TERT over-activation at all. If we could trap TERT mRNA in the nucleus, it wouldn’t matter how much of it there is—without the ability to reach ribosomes in the cytoplasm, the TERT gene wouldn’t be manufactured into the telomerase enzyme.
In fact, Cech’s lab discovered the action of the TERT gene in cancer nearly 22 years ago.
“At the time, it was just a basic science discovery. We weren’t working on cancer, just interested in this little machine,” he says. “Time went on and now several hundred labs around the world are working on TERT.”
One thing these labs agree on is that TERT is a major cancer-causing gene. They see TERT over-activation and the accumulation of telomerase in cancer cells. But labs had never looked at the timeline of this telomerase accumulation. Here’s where this science story becomes a people story.
“Two years ago, John Rinn moved his lab to our institute from Harvard. One of his postdocs, Gabrijela Dumbovic, struck up conversations with a postdoc in my lab, Teisha Rowland [first author on the current paper]. Gabby had the ability to see RNA in individual cells and even track the movement over time of specific RNA molecules. The result is this collaboration: We can see RNA spewing out from the TERT gene as it’s being made, and we can also see individual mRNA molecules moving from the nucleus to the cytoplasm,” Cech says.
What they saw is that while all other messenger RNAs move quickly from nucleus to cytoplasm, TERT messenger RNA is held up in the nucleus.
“It’s not that none of it gets out. It’s like half gets out. It’s like a flipbook: At the first snapshot, we can see RNA being made at the TERT gene. Then as we flip through later snapshots, we see, surprisingly, a lot of it still stuck in the same compartment it’s made, even after days. Some gets out, but a lot appears to be stuck. Keeping TERT RNA trapped in the nucleus would be just as good as knocking out the gene—if it were stuck in the nucleus, it couldn’t do anything,” Cech says.
However, Cech also cautions that TERT-trapping isn’t ready for primetime. In addition to better understanding the mechanism that keeps TERT messenger RNA trapped in the nucleus and designing/testing a way to magnify or manipulate this effect, is the major challenge that some telomerase is important for the function of the body’s healthy cells, especially stem cells. Completely erasing the action of TERT would be, as scientists say, a bad thing.
“Unfortunately, it’s a double-edged sword. If telomeres get too short, you get genome instability, which is another hallmark of cancer. You need TERT action in a Goldilocks range—not too hot, not too cold. Just the right telomeres,” Cech says.
“It took 22 years to go from the discovery of the TERT gene to this finding,” he says. “We hope it’s not another 22 years before we find a way to act against TERT in cancer.”

