Seniors who suffered a ‘silent stroke’ after surgery faced double the risk of dementia or further strokes than those patients who did not have a stroke, according to a recent Western-led international study. These findings open the door to revolutionizing stroke care and prevention for millions of patients.
“Although we know stroke affects cognitive function, it was still surprising that it created this toxic stew where it doubled the risk of delirium,” explained Dr. Marko Mrkobrada, a Schulich School of Medicine & Dentistry professor and co-principal investigator of the NeuroVISION study. “It is very surprising that something so small could have such a profound affect.”
The study, “Perioperative covert stroke in patients undergoing non-cardiac surgery (NeuroVISION): a prospective cohort study,” was recently published in the medical journal The Lancet.
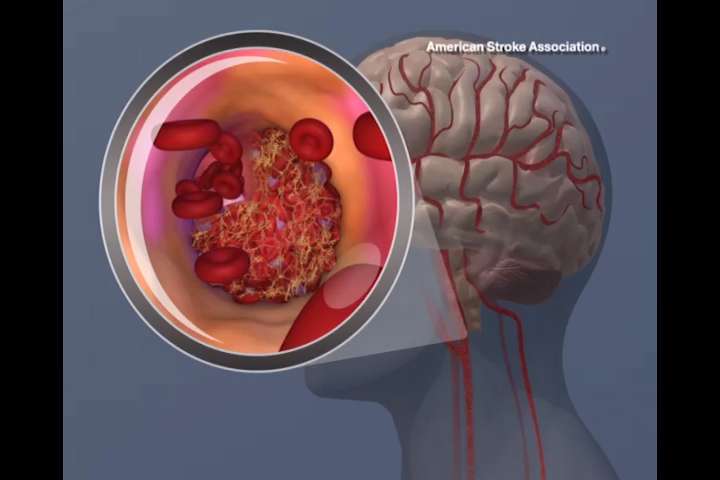
When people think stroke, they usually picture what is known as an overt stroke—recognizable from paralysis that occurs in the face, arm or leg, often just on one side of the body. These strokes are fatal within 90 days in 13 percent of patients.
A silent stroke—officially known as a covert stroke—is far more difficult to detect as there are no obvious immediate physical damage and does not affect muscle or motor skills. However, it occurs five times more often than overt strokes and can be far more deadly.
In a surgery setting, those numbers mean a lot.
“If you look at patients who are having surgery and they have a stroke, their mortality rate is about 30 percent,” Mrkobrada explaining, noting half of the surviving patients will end up in a nursing home. “We’ve established the fact the injuries we’re seeing to the brain has real and measurable consequences. This is clinically significant.”
NeuroVISION involved 1,114 patients aged 65 years and older (who underwent inpatient, elective, non-cardiac surgery and had brain MRI after the operation. They were drawn from 12 academic centres in nine countries (Canada, Chile, China, India, Malaysia, New Zealand, Peru, Poland, and the United States).
Non-cardiac surgery was studied because it does not affect the blood supply to the brain.
The research team followed patients for one year after surgery to assess cognitive capabilities. They found those who had a silent stroke during that time were at double risk to experience cognitive decline, perioperative delirium and an overt stroke or transient ischemic attack within the year, than those who did not have a stroke.
“These silent strokes were much more serious than overt strokes. Why is that? Is it that strokes after surgery are so much more different than not after surgery? Or is it strokes after surgery are much more severe because we are missing a large proportion of very, very small strokes that we’re not picking up?”
For example, if someone has a hip operation and can’t move their hip or leg due to a silent stroke, they’re likely not going to complain about it, assuming its part of the surgery. Or if they’re slurring their words, perhaps they assume it’s the pain medication and it will go away.”
Mrkobrada continued, “What we found was there are these silent strokes. But the question is, “Are they truly silent?” Around surgery, it’s a time of stress, both physiological and emotional. There are changes in blood pressure. There’s clotting. There are inflammations, different kinds of heart rhythms.
“It’s probably a combination of all these things that are going on that’s triggering this. Anesthetic and surgical techniques have improved substantially, and we’re operating on older and older people. No question surgery is getting safer and safer. But having said that it’s still a huge stress to the system.”
Moving forward, Mrkobrada looks to determine the cause of the strokes and, more importantly, how to deal with them. His next research project, NeuroVISION 2, will explore heart rhythms and blood pressure during surgeries in an effort to spot potential bio-marker for strokes.
“Is it blood pressure going really high and low during surgery? We can we control that. Is it bad heart rhythms, like atrial fibrillation? If we’re able to prevent that, or potentially put people on extra blood thinners, could that be it? This would revolutionize stroke care.”
Source: University of Western Ontario

