Researchers at Carnegie Mellon University have discovered that the spreading of seizures through the brain can be suppressed depending on the amount of pressure within the brain, an important discovery that may revolutionize the treatment of drug-resistant epilepsy.
Epilepsy is one of the most common neurological diseases, affecting people of all ages. There are many seizure disorders, all of which fall under the umbrella of epilepsy. While many seizure disorders can be treated with medication, some patients have strains of epilepsy that are resistant to drugs, meaning that sometimes surgical intervention is necessary. In these patients, tissue can be surgically removed to eliminate or minimize future seizures.
The lab of Department Head of Biomedical Engineering Bin He, in collaboration with Mayo Clinic, has published a study in the journal Annals of Neurology that finds that within the brain, “focal seizures”—seizures that originate at a single point—can be regulated by push-pull dynamics within the brain.
The paper, “Multiple Oscillatory Push-Pull Antagonisms Constrain Seizure Propagation,” further shows that an imbalance of excitation-inhibition activity within an epileptic network may be a promising biomarker for the secondary generalization of focal seizures. In other words, when medical professionals see indications that the excitation and inhibition of neuron firing within the brain is imbalanced, this imbalance may be an indicator as to if the seizure will propagate in the brain.
“People thought that the spread of seizures mainly depends on where seizures originate in the brain, but the propagation of a seizure is actually regulated by the surrounding tissues, which includes that seizure onset zone,” says He. “By using an array of electrophysiological recordings, we found that it’s not moving outward necessarily; it depends on how much ‘pull’ a patient receives from the surrounding tissue towards the seizure onset zone, and how much ‘push’ propagates from seizure onset zone in the same patient. If that pull is weak, then it’s going to spread. If that pull is strong, then we can contain the seizure where it is and prevent it from spreading.”
Although drug-resistant focal epilepsy is widely recognized among medical professionals to be a network disease (i.e. a seizure spreads through the brain after originating from a single point) in which seizures propagate in coordination with different neuron oscillation frequencies, the mechanism by which different networks constrain the spreading of focal seizures remains unclear.
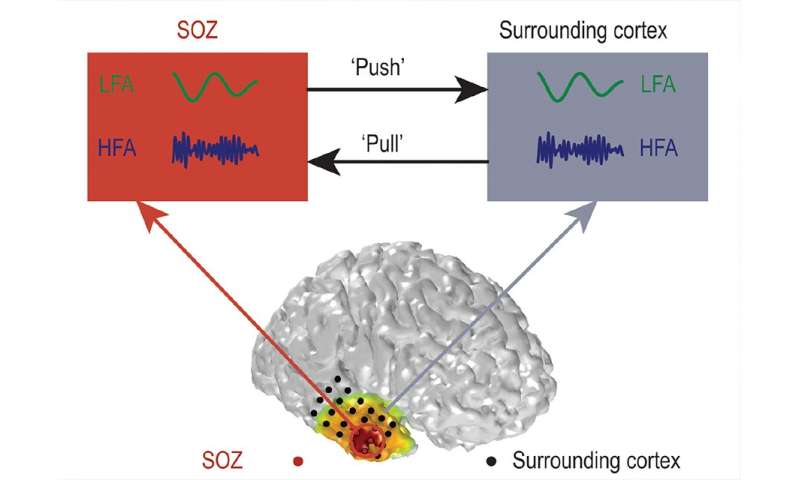
In the work by He and his team, researchers tackle the problem by looking at various frequencies, including both slow and fast brain rhythms. They further performed novel analysis of functional networks for a given rhythmic band, or the interactions between low and high brain rhythms. By using a novel “cross-frequency directionality” technique to study 24 focal drug-resistant epilepsy patients, the team found that the propagation of seizures through the brain depend on a “push-pull” antagonism control mechanism. This “push-pull” mechanism can potentially reflect connections in the epileptic network, suppressing the seizure.
“This finding will have important implications, and suggests that future treatment options should consider interventions not only upon seizure onset zones, but also the surrounding tissues,” says He. “Further delineation of critical network nodes may assist the development of treatments for epilepsy using neuromodulation.”
Source: Carnegie Mellon University