Blood clotting in veins, a disorder called venous thromboembolism (VTE), is a common vascular disease like heart attack and stroke, but hasn’t been as well studied. Genetics are known to be involved, but only about a dozen genomic regions have been linked with the condition. Now a large genetic study of VTE led by researchers at the Broad Institute of MIT and Harvard, Massachusetts General Hospital (MGH), and the US Department of Veterans Affairs (VA) Boston Healthcare System has found 22 new regions in the genome that contribute to the disease. The team has also developed a genetic score that could one day be used to identify patients at highest risk for the disease.
A more accurate way of predicting who’s at increased risk could better ensure that only the highest risk patients receive preventative treatment for VTE, namely blood-thinning drugs, which can predispose patients to excessive bleeding.
The study, published in the November 2019 issue of Nature Genetics, analyzed genetic data from more than 650,000 people and found 33 locations in the genome—22 not previously known— that may play a role in the disease. The team also revealed some genetic overlap with other forms of vascular disease, an insight that could help spark the development of new, safer treatments.
“Our study represents a significant step forward in genetic discovery for VTE, both in terms of the number and diversity of individuals we studied as well as the number of genetic variants we identified that were linked to VTE,” said senior author Pradeep Natarajan, an associate member at the Broad Institute and director of preventive cardiology at MGH.
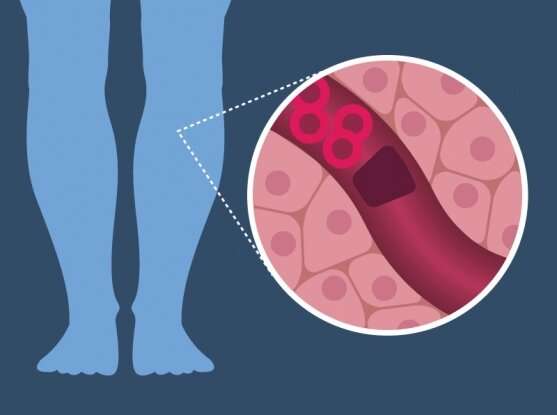
Lurking in veins
In VTE, blood clots form in the deep veins, often in the legs. They can then dislodge and become potentially fatal if they travel through the bloodstream to the lungs. Smoking, cancer, pregnancy, prolonged sedentary periods, as well as a recent hospital stay are all associated with VTE. In the U.S. alone, more than 500,000 hospitalized adults develop the disorder each year.
Previous studies have uncovered a handful of genetic variants associated with VTE. Two in particular—one in the gene for a blood-clotting factor called Factor V and the other in the prothrombin gene—each increase VTE risk two- to three-fold and are found in roughly 1 to 3 percent of the population.
To search for more VTE genomic regions, Natarajan and his colleagues conducted a genome-wide association study (GWAS). The researchers, which include first author Derek Klarin of the Broad Institute, the VA Boston Healthcare System, Massachusetts General Hospital, and the University of Florida School of Medicine, and co-senior author Scott Damrauer of the Corporal Michael Crescenz VA Medical Center and the University of Pennsylvania’s Perelman School of Medicine, studied data from two large-scale biobanks: the UK Biobank and the Million Veteran Program. Their initial analysis spanned approximately 13 million DNA variants and 650,00 individuals, including VTE patients and healthy controls. To validate their findings, the researchers also used a third collection of more than 180,000 samples from VTE patients and disease-free controls from the INVENT consortium.
Of the newly discovered genomic regions linked to VTE, many are located in or near genes associated with blood clotting. Other regions have unknown roles.
Risk predictor
To try to predict who will more likely develop VTE, the researchers developed a polygenic risk score, which they calculated based on the risk contributed by nearly 300 genetic variants. They excluded the known VTE risk factors in the Factor V and prothrombin genes from their calculations to see if they could identify more high-risk patients based on genetic predisposition. The team then tested this score using additional data from the Million Veteran Program as well as the Women’s Health Initiative.
The polygenic score flagged 5 percent of the study population as having a two- to three-fold increased risk for VTE. These people have a similar level of risk as those with either the Factor V Leiden or the prothrombin mutations—but represent a larger group, suggesting that polygenic scores could potentially identify more patients as genetically high-risk for VTE than current methods.
Natarajan emphasizes that his team’s polygenic score is a research tool and requires further study before it can be used clinically.
He and his colleagues also found that some of the genetic variants linked to VTE are the same as ones associated with other vascular conditions such as coronary artery disease, peripheral arterial disease, and stroke. This finding may explain why LDL cholesterol-lowering drugs called statins, which effectively lower heart disease risk, have been shown to decrease VTE risk in secondary analyses of some statin clinical trials.
“I think there is an important opportunity here for future work, especially with the genetic variants that overlap all of these conditions, to develop maximally efficient therapies that work for multiple disorders,” said Natarajan. “That might involve anti-coagulation, or even safer strategies such as lowering LDL cholesterol.”
Nicole Davis, Broad Institute of MIT and Harvard

