People with prosopagnosia, or “face blindness,” have trouble recognizing faces—even those of close friends and family members. It often causes serious social problems, although some people can compensate by using clothing and other cues. Face blindness often becomes apparent in early childhood, but people occasionally acquire it from a brain injury later in life. A new study of people who became face-blind after a stroke, led by Alexander Cohen, MD, Ph.D., of Boston Children’s Hospital, provides clues to what goes wrong in the brain.
The findings, published in the journal Brain, indicate that no one single area is always perturbed in face blindness. Instead, face blindness involves an entire network, where a malfunction in communication among the various components can bring the system down.
This potentially opens the door for improving face recognition by tweaking the function of different parts of the network.Cohen, first author on the paper, believes the findings could also apply to other people with poor face-processing abilities, specifically individuals with autism, who often score very poorly on tests of face processing.From autism to stroke and back againCohen began by speculating that autism could be approached not just as a holistic entity, but by studying its individual symptoms.
Those symptoms have a better chance of being localized to specific parts of the brain and could perhaps be turned into biomarkers and treatment targets.That’s where face blindness comes in. It’s easy to test for and common in autism, seen in children as young as 2.”In eye gaze studies, autistic kids often don’t look at the faces in a video,” Cohen says “Or they just look at one part, often the mouth, maybe because it’s giving more information about speech. Many find eye contact uncomfortable.
“Data suggest that the worse people with autism are at face processing, the worse their social communication. “The question is, are face processing deficits causal in autism, or do they result from autism?” says Cohen. “That’s where looking at face processing in people with stroke really helps. They have specific lesions in the brain, so there is more of a cause-and-effect relationship. If you find an abnormality involving the same brain areas in a child with autism, there’s a much higher chance that it may be driving the face processing deficit.”
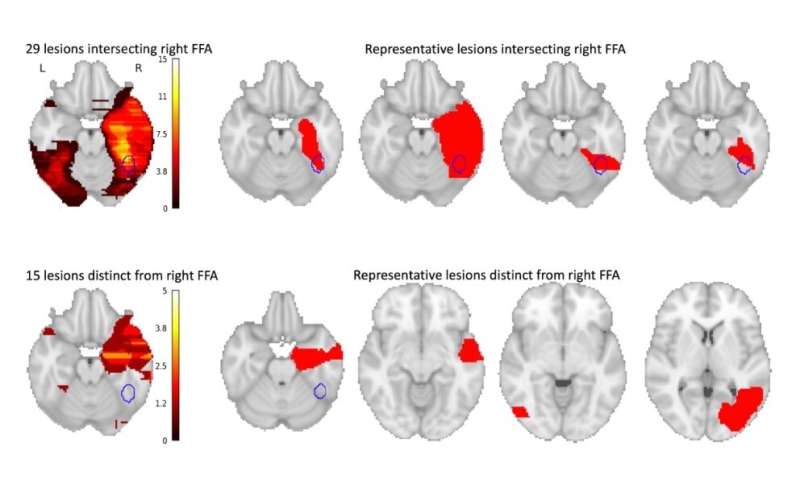
Mapping brain networksFace blindness has previously been linked to the brain’s right fusiform face area (FFA), but not everyone with face blindness shows damage there. Cohen searched the medical literature and identified 44 people from 19 studies who developed face blindness after a stroke and who also had brain MRI data available. Of the 44 lesions causing face blindness, only 29 involved the right FFA; the other 15 did not.
To try to explain these cases, Cohen used a new method, developed by senior study author Michael Fox, MD, Ph.D., of Beth Israel Deaconess Medical Center, that draws on data from functional MRI images to create a large-scale map of brain networks, showing the relationships between different brain areas. With it, Cohen could determine which networks were consistently injured in the stroke patients that developed face blindness.
The 15 lesions that did not involve the FFA, Cohen’s team found, were in areas that were functionally connected to the right FFA, meaning that they are typically used when the FFA is being used, and become quiet when the FFA is quiet.Surprisingly, all 44 lesion locations were also negatively connected with four additional areas in the left frontal cortex—meaning that brain activity in the four areas goes down when activity in the lesion locations goes up, and vice versa.
Intriguingly, all four of the new areas belong to the left frontoparietal control network, which attends to specific features of a visual stimulus. Based on the findings, Cohen speculates that face recognition involves two distinct brain networks. It’s not yet clear whether face blindness results from both networks being disrupted, or from an imbalance between the two. “Maybe in face blindness, you’re using too much detail information, and are not looking at the face as a whole,” Cohen says. “That exact imbalance is something that has been seen in autism.
Or, maybe you need both kinds of information to recognize a face.”Mapping face processing in tuberous sclerosisBased on the stroke data, Cohen now plans to delve back into face processing problems in autism spectrum disorder. Under a $100,000 two-year research award from the Child Neurology Foundation, Cohen will study children with tuberous sclerosis complex (TSC), a genetic syndrome that often includes autism and atypical face processing.Most children with TSC have tubers (noncancerous tumors) in their brains that are thought to affect the function of nearby brain tissue. To see if they have any relationship with face processing, Cohen will recruit up to 80 children with TSC, locate their brain tubers, administer tests of face processing, and map their brain networks. He will then compare the findings with his data from the stroke study to see if common brain areas are involved.
Could face blindness be treated?Eventually, Cohen hopes to do a larger study of brain connectivity and face processing in children with garden-variety (non-syndromic) autism. “Just as many disorders can be affected by multiple genes, it may take a whole network of brain regions to cause a symptom,” he says.If all roads in that network lead to a specific area in the brain, that area could potentially be treated by methods to increase or decrease its activity. Even addressing face processing in isolation could improve the quality of life in children with autism—and others with face blindness.”We could try to modulate activity in that spot—with novel therapies like transcranial magnetic stimulation or functional-MRI-based neurofeedback—and see if it affects behavior,” Cohen says. “If this works, we aim to expand this methodology to many other symptoms in autism as well.”
Children’s Hospital Boston

