Dying cells in the body can keep the immune system in check, thus preventing unwanted immune responses against the body’s own tissues. Scientists from the German Cancer Research Center have now identified a receptor on murine immune cells that activates this protective mechanism and can thus prevent dangerous autoimmune reactions in which the immune system attacks the patient’s own body tissues.
Billions of cells die every day in the human body. This occurs as part of a highly regulated process called apoptosis or programmed cell death. The dying cells confront the immune system with large amounts of proteins, which ought to activate an immune response, but the apoptotic cells seem to actively suppress the immune system so that it does not attack the body’s own tissues. “We began wondering many years ago what kind of protective mechanism prevents autoimmune reactions – the body attacking its own tissues – when cells in the immune system, such as dendritic cells, take up the remains of the dead cells,” Peter Krammer, an immunologist at the German Cancer Research Center (DKFZ), remarked.
Krammer, his colleague Heiko Weyd, and their team recently found an answer to the question: As soon as apoptosis is triggered, the dying cells transport proteins from the annexin family to the cell surface. The annexins act like a stop signal for the cells of the immune system and prevent an immune response from being triggered.
Kevin Bode from Krammer’s department has now identified the dectin-1 protein as the annexin-binding receptor on the surface of dendritic cells: Dectin-1 recognizes the annexins and triggers a signaling pathway in dendritic cells that ultimately suppresses the immune response.
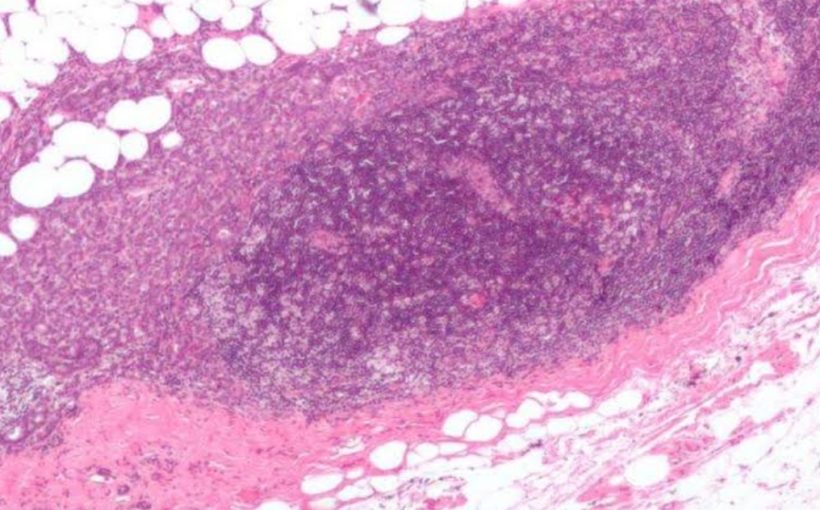
Mice that do not have any dectin-1 on the surface of their dendritic cells showed a stronger immune response to dying, apoptotic cells. Moreover, the mice without dectin-1 developed signs of autoimmune diseases in old age.
The DKFZ scientists thus discovered an important control mechanism for the immune system’s ‘self-tolerance’. “But we assume that the body has other protective functions to prevent autoimmune reactions too. That’s why the loss of dectin-1 in the animals does not become apparent until later in life,” Bode explained.
“Interestingly, dectin-1 has a dual role,” added Peter Krammer. Dectin-1 not only binds annexins; it also binds certain pathogens at a different binding site. This has the opposite effect and triggers an immune response. “We thus identified a crucial immune checkpoint which, depending on the binding partner, either triggers or suppresses the immune response,” Krammer explained, emphasizing the importance of the work.
A key link in the dectin-1 signaling pathway is the enzyme NADPH oxidase 2. People who lack this enzyme develop autoimmune diseases. In cooperation with the Children’s Hospital Zurich and Heidelberg University Hospital, the DKFZ researchers are therefore currently examining blood samples from patients lacking NADPH oxidase 2 to find new starting points for potential treatments.
Why animal experiments are vital in cancer research
Autoimmune diseases have a hugely detrimental impact on patients’ lives and in some cases are even life-threatening. In order to develop effective treatments, it is therefore vital to know which mechanisms suppress the immune responses to a patient’s own body tissues or in contrast activate them. By establishing the interaction between annexin on the surface of dying cells and dectin-1 on the dendritic cells, Bode and his colleagues identified a key mechanism that prevents autoimmune reactions in healthy body tissues. In doing so, they have found an interesting starting point for future drug treatments.
Although the interactions between annexin and dectin-1 were initially identified in a Petri dish, the scientists needed an animal – with all the diversity of the various components of the immune system – to demonstrate that the bond between these two proteins actually suppresses autoimmune reactions.
GERMAN CANCER RESEARCH CENTER (DEUTSCHES KREBSFORSCHUNGSZENTRUM, DKFZ)