Artificial intelligence can help cancer patients start their radiation therapy sooner—and thereby decrease the odds of the cancer spreading—by instantly translating complex clinical data into an optimal plan of attack.
Patients typically must wait several days to a week to begin therapy while doctors manually develop treatment plans. But new research from UT Southwestern shows how enhanced deep-learning models streamlined this process down to a fraction of a second.
“Some of these patients need radiation therapy immediately, but doctors often have to tell them to go home and wait,” says Steve Jiang, Ph.D., who directs UT Southwestern’s Medical Artificial Intelligence and Automation (MAIA) Lab. “Achieving optimal treatment plans in near real time is important and part of our broader mission to use AI to improve all aspects of cancer care.”
Radiation therapy is a common form of cancer treatment that utilizes high radiation beams to destroy cancer cells and shrink tumors. Previous research shows that delaying this therapy by even a week can increase the chance of some cancers either recurring or spreading by 12-14 percent.
Such statistics motivated Jiang’s team to explore methods of using AI to improve multiple facets of radiation therapy—from the initial dosage plans required before the treatment can begin to the dose recalculations that occur as the plan progresses.
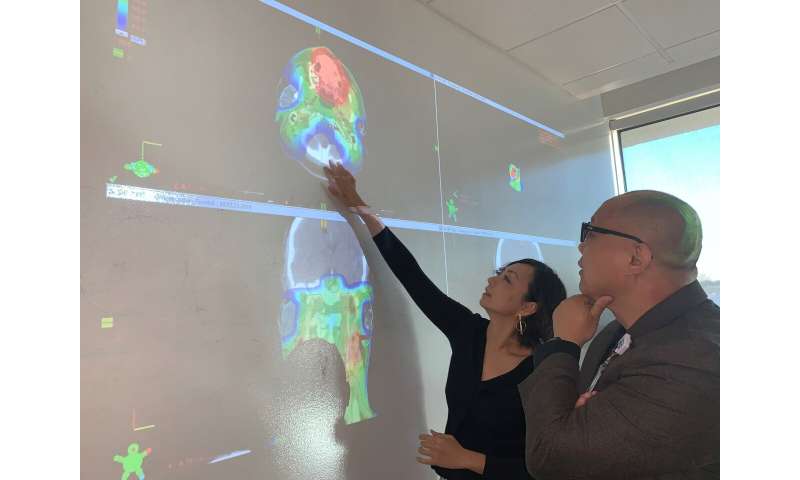
Jiang says developing a sophisticated treatment plan can be a time-consuming and tedious process that involves careful review of the patient’s imaging data and several phases of feedback within the medical team.
A new study from the MAIA Lab on dose prediction, published in Medical Physics, demonstrated AI’s ability to produce optimal treatment plans within five-hundredths of a second after receiving clinical data for patients.
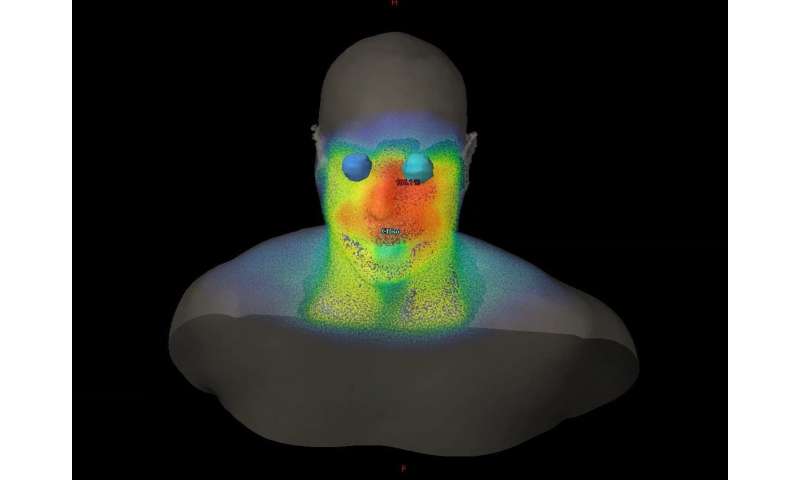
Researchers achieved this by feeding the data for 70 prostate cancer patients into four deep-learning models. Through repetition, the AI learned to develop 3-D renderings of how best to distribute the radiation in each patient. Each model accurately predicted the treatment plans developed by the medical team.
The study builds upon other MAIA research published in 2019 that focused on developing treatment plans for lung and head and neck cancer.
“Our AI can cut out much of the back and forth that happens between the doctor and the dosage planner,” Jiang says. “This improves the efficiency dramatically.”
A second new study by Jiang, also published in Medical Physics, shows how AI can quickly and accurately recalculate dosages before each radiation session, taking into account how the patient’s anatomy may have changed since the last therapy. A conventional, accurate recalculation sometimes requires patients to wait 10 minutes or more, in addition to the time needed to conduct anatomy imaging before each session.
Jiang’s researchers developed an AI algorithm that combined two conventional models that had been used for dose calculation: a simple, fast model that lacked accuracy and a complex one that was accurate but required a much longer time, often about a half-hour.
The newly developed AI assessed the differences between the models—based on data from 70 prostate cancer patients—and learned how to utilize both speed and accuracy to generate calculations within one second.
UT Southwestern plans to use the new AI capabilities in clinical care after implementing a patient interface. Meanwhile, the MAIA Lab is developing deep-learning tools for several other purposes, including enhanced medical imaging and image processing, automated medical procedures, and improved disease diagnosis and treatment outcome prediction.
Southwestern Medical Center


