Clinical observations of COVID-19 patients, who went on to have a stroke, suggest coronavirus may cause clots within blood vessels (arteries) in the brain, finds a team of neurologists from UCL and UCLH (the National Hospital for Neurology and Neurosurgery), London.
The findings suggest early testing for D-dimer, a protein fragment in the blood associated with increased blood clotting (thrombosis) in COVID-19 patients, could enable clinicians to prescribe specific treatments, including anticoagulants (“blood thinners”), at a much earlier stage, which might reduce the number of people subsequently having further strokes or blood clots elsewhere in the body.
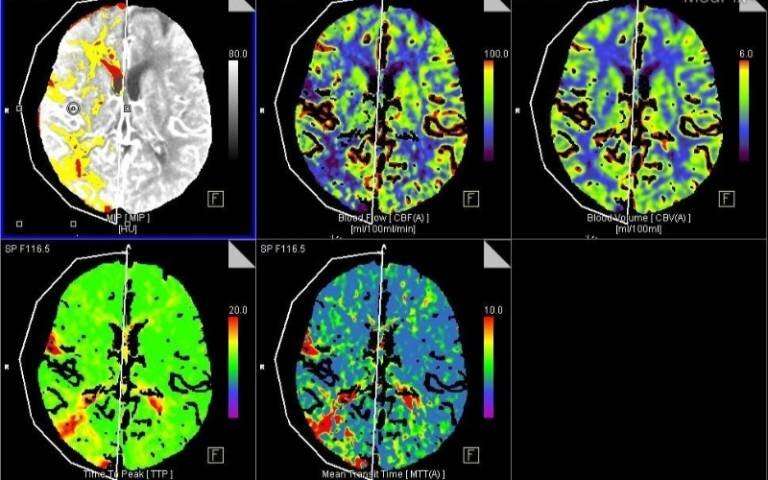
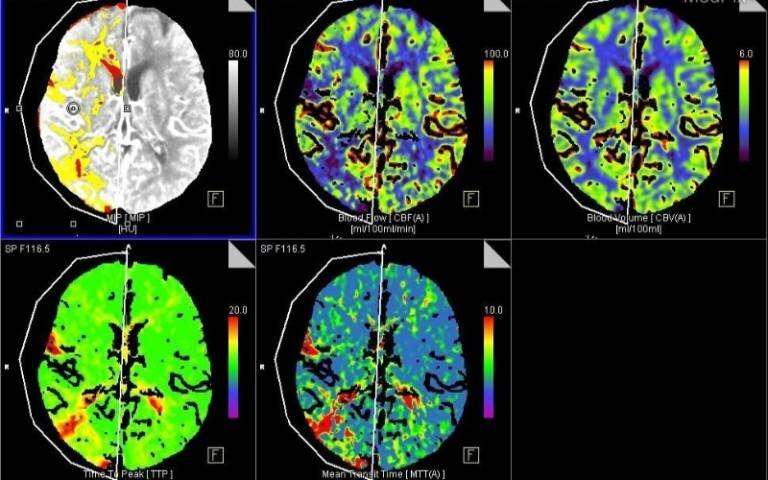
In a research article published in the Journal of Neurology, Neurosurgery, and Psychiatry, corresponding author Professor David Werring (UCL Queen Square Institute of Neurology) and colleagues report on six consecutive patients assessed between April 1 to 16 2020 at the National Hospital for Neurology and Neurosurgery, London, (part of University College London Hospitals NHS Foundation Trust) with acute ischaemic stroke (due to blockage of a large brain artery) and proven COVID-19. Acute ischaemic stroke is caused by the sudden loss of blood circulation to an area of the brain, resulting in loss of neurological function.
In summary, all six patients (aged between 53 and 85) had large vessel occlusion (large arterial blockage), with markedly elevated blood levels of D-Dimer indicating the presence of abnormally high “fibrin degradation products”—components in the blood produced when clots break down.
This report is based on a small number of patients, and doesn’t confirm a direct link between COVID-19 and stroke (as other factors that are linked to stroke were present in most patients). However, the findings support other recent evidence: the exaggerated inflammatory immune response known to occur in COVID-19 patients stimulates abnormal blood coagulation, including raised D-dimer and the production of antiphospholipid antibodies—which are usually caused by a disorder in the immune system.
Furthermore, five of the six ischaemic strokes occurred 8-24 days after COVID-19 symptom onset (cough, headache, and chills), and in one patient during the pre-symptomatic phase, suggesting that COVID-19 associated ischaemic stroke is usually delayed, but can occur both early and later in the course of the disease.
Discussing the findings, Professor Werring, Professor of Clinical Neurology at UCL and a Consultant Neurologist at the National Hospital for Neurology and Neurosurgery, Queen Square, London, said: “We now know that COVID-19 is not just a disease of the lungs. Our findings suggest that blockages of large brain arteries in COVID-19 patients are associated with highly abnormal blood clotting.
“Early use of anticoagulant drugs might be helpful, but this needs to be balanced against their brain bleeding risk, especially soon after an ischaemic stroke.
“Clinical studies (ideally controlled trials) are needed to find out the best treatment to reduce the disability caused by ischaemic stroke in people with COVID-19. Our findings emphasise that even during the lockdown people with suspected stroke must attend hospital immediately to ensure they get the best treatment.”
Henry Killworth, University College London