As a rubber-like elastic tissue with widely varying properties, cartilage lubricates joints to keep them healthy and in motion, and forms many of our internal structures, such as the intervertebral discs in the spine, the flexible connections between ribs, and the voice box, as well as external tissues like noses and ears.
Specifically, in joints, the wear-and-tear of cartilage over time can eventually result in the painful bone-on-bone contacts, and the bone damage and inflammatory reactions that plague patients with osteoarthritis, the most common form of arthritis. In the U.S. alone, 32.5 million adults are affected by osteoarthritis, and thus far, there is no strategy that allows lasting repair or replacement of degenerating joint (articular) cartilage.
To overcome this problem, researchers are using tissue engineering strategies to generate cartilage from stem cells outside of the human body. However, according to Eben Alsberg, Ph.D., at the University of Illinois in Chicago,”It can be challenging to prevent fibrocartilage and hypertrophic cartilage from forming when using tissue engineering strategies.” Upon implantation into joints, engineered cartilage can become unstable and dysfunctional, and methods that can determine more complex conditions for the production of high-quality cartilage ex vivo and its maintenance in vivo thus far were limited.
Now, a collaborative research team led by Ali Khademhosseini, Ph.D., the director and CEO of the Terasaki Institute, has developed a multi-component biomaterial-based screening approach that identifies material compositions, and mechanical and molecular stimuli enabling human stem cells to differentiate into cells capable of generating higher-quality articular cartilage. The study is published in Science Advances.
“We took a holistic approach to cartilage engineering with this multicomponent in vitro approach by screening with high-throughput through many combinations of material, biomechanical and molecular parameters, which in this complexity had not been done before,” said Khademhosseini. “This allowed us to define material properties and compositions, and specific mechanical, biochemical, and pharmacological contributions that help guide human mesenchymal stem cells (hMSCs) down a differentiation path towards articular cartilage-producing chondrocytes in vitro, and better maintain their functionality when transferred into mice.”
Chondrocytes, which are differentiating from hMSCs, form cartilage by secreting collagen and other biomolecules into their extracellular environments where they form a hydrated elastic matrix. However, as differentiated cartilage only retains relatively low numbers of normally functioning chondrocytes, and lacks supportive blood vessels, it cannot efficiently repair and regenerate itself.
In the study, the team assembled a compression bioreactor from 3-D printed components with an array of 288 individual hydrogel-based biomaterials for screening of multiple parameters presented in the native developing cartilage microenvironment. These hydrogels were made up of two different biomaterials, oxidized methacrylated alginate (OMA) and polyethylene glycol (PEG). The two hydrogel components can be cross-linked to each other to create a biodegradable and biocompatible dense interconnected elastic network. Within the biomaterial, the researchers embedded hMSCs, as well as cell-binding ligands that mimic the normal extracellular environment of developing cartilage, and growth factors favoring cartilage cell differentiation. The hydrogel biomaterial with the encapsulated hMSCs could be mechanically manipulated between fixed and movable plates, whereby the movable plate is cyclically pushed up from the bottom with finely calibrated forces, causing the biomaterial scaffold to be compressed and then relaxed again each time.
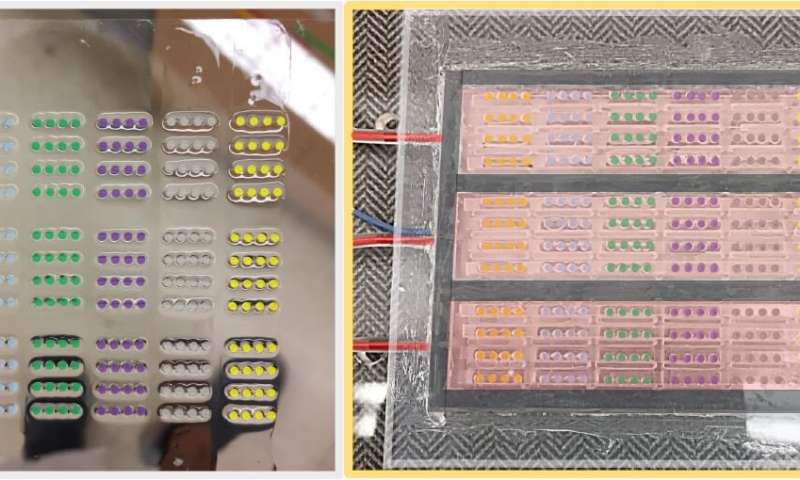
To be able to support the hMSCs with cartilage-specific cell culture medium and expose them to additional biochemical cues while they differentiate, the device was separated into multiple chambers, each linked to a microfluidic support system. Since all relevant biomaterial, mechanical and chemical parameters could be individually varied between biomaterials of the array, the researchers could study multiple combinations of cues simultaneously.
“Our approach pinpointed biomaterial compositions that provided a sweet spot of hydrogel physical properties, just the right amounts of extracellular matrix and critical growth factors, and mechanical stimulation that hMSCs needed in this complexity to develop into highly functional articular chondrocytes in the engineered system,” said co-first author Junmin Lee, Ph.D., a postdoctoral fellow in Khademhosseini’s group.
Alsberg added that the team’s device-driven biomaterials strategy “identified cues in the cellular microenvironment that could preferentially drive engineered tissue constructs to a preferred hyaline cartilage phenotype.” Chondrocytes that matured in the biomaterials secreted substantial amounts of extracellular matrix molecules that compose natural joint cartilage.
Lee and the other co-first author Oju Jeon, Ph.D., a research professor working with Alsberg, and additional team members, also studied molecular pathways that chondrocytes normally use to transduce mechanical signals from their extracellular environment to control their gene expression. “We found that suboptimal biomaterial properties that elevated the activity of a mechanotransducing protein called YAP and its downstream effects were causing chondrocytes to adopt a less functional state strongly resembling the one in hypertrophic cartilage in patients,” said Jeon. “In contrast, inhibiting YAP with a specific drug favored the formation of functional articular chondrocytes in our system.”
The YAP inhibitor as well as an inhibitor of WNT, another protein involved in mechanotransduction, were also found by the team in a search for drugs that would favor the formation of healthy articular cartilage in their system.
To investigate whether their overall approach could enable the generation of chondrocytes that would also be more effective in vivo, they scaled up a successful condition that resulted from their screening procedure from a hydrogel 1 mm in diameter to one that measured 8 mm in diameter. “When we actively inhibited YAP or the mechanical signal transducer WNT during 21 days of chondrocyte differentiation in vitro, implanted the engineered tissue under the skin of mice, and analyzed the implants again after an additional 21 days, we observed higher-quality chondrocytes with significantly less hypertrophy compared to controls that were not treated with inhibitors prior to implantation,” said Jeon.
“The opportunities that our approach offers and the information it already helped us provide is an important step towards the generation of truly therapeutic articular cartilage, and some of the insights we gleaned could also be tooled for enhancing the function of existing joint cartilage in patients with osteoarthritis and for more personalized strategies,” said Khademhosseini. His group continues their efforts at the interface of the Terasaki Institute’s Personalized Implants, Personalized Cells, and Personalized Materials platforms in collaboration with the Alsberg Stem Cell & Engineered Novel Therapeutics (ASCENT) Laboratory.
Terasaki Institute for Biomedical Innovation