Developing a vaccine is difficult at the best of times, but rarely have we been in a situation where basic knowledge about a virus has to be acquired so directly alongside the race to eradicate it. To understand how difficult this task is, we must appreciate the complexity of how our immune system responds to an infection.
The part of the immune response that can target germs precisely and provide long-term protection is called the adaptive immune response. Two types of white blood cell are important in this: T cells and B cells. These cells work together to orchestrate a targeted immune response. But the way they recognise and deal with germs is different.
Both T cells and B cells have an important receptor molecule on their surface, not so imaginatively called the T cell receptor and the B cell receptor. B cell receptors lock onto unique structural components of a germ, or an infected cell, directly. T cells, on the other hand, need other immune cells to chew up and present parts of the germ in small fragments, which can then be scrutinised.
So for any given germ, T cells and B cells see it differently. They also respond in different ways. Even T cells don’t just do one thing. Some—the cytotoxic T cells—attack infected cells directly, while others—the T helper cells—support immune responses by helping B cells produce antibodies.
All this complexity serves to attack different germs in different ways and helps prevent unintended damage to our body’s healthy cells and tissues, as it provides multi-step checks before an immune response is fully activated.
Getting T cells and B cells to respond to a germ takes time—usually several days following the initial infection. Once T and B cells have been sent to deal with a germ, the immune response subsides and long-lived memory versions of T cells and B cells are retained so that the appropriate response can be mounted much faster if the same germ is encountered again.
Vaccines try to mimic this natural process by provoking the development of long-lived memory T cells and B cells, without triggering the symptoms of a real infection. It’s not the case, though, that each type of vaccine stimulates a similar immune response. There are many types of vaccine and each will trigger a cascade of events that stimulate the immune system in a particular way.
Most vaccines will target B cells and the types of T cells that support antibody production. Yet for some infections, the antibody response may not be enough. In such cases, vaccines can also be developed to promote cytotoxic T cell activity, or perhaps a combination of both antibody and cytotoxic T cell immune responses.
Understanding the type of immune response that works best against a particular infection is important for vaccine design. And we are still learning about our adaptive immune response to the novel coronavirus.
Looking beyond spike proteins
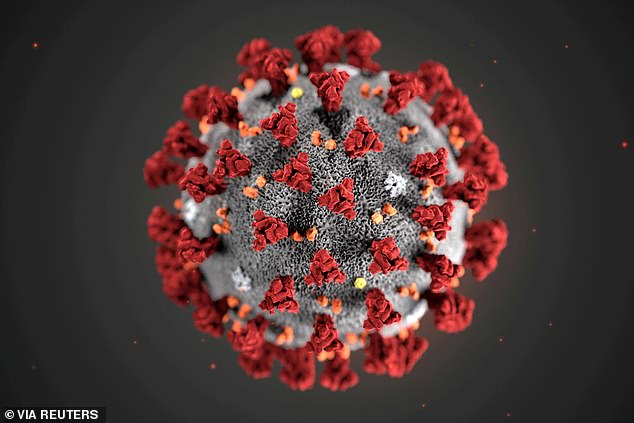
The virus can be pictured as a small spiky ball that encapsulates genetic material. Many vaccines currently being tested aim to create an immune reaction against the protein molecules that make up the outer spikes. The spikes are critical for how the virus gets into human cells, so antibodies that lock onto those structures might stop the virus from entering cells. But the evidence is mounting that targeting other parts of the virus might also be useful.
A recent study—which has yet to be peer-reviewed—assessed T cell memory responses in patients who had recovered from mild and severe COVID-19. Patients who had severe symptoms showed a stronger and more varied T cell response. Their T cells reacted to the virus’s spikes, but also to internal components of the virus—which have cumbersome names such as “receptor binding domains” and “nucleoproteins”.
In detail, cytotoxic T cells that could attack virus-infected cells directly seemed to target internal parts of the virus, whereas T helper cells, which support antibody production, reacted to viral surface molecules.
Having an immune response capable of detecting different aspects of a virus might make it harder for the virus to escape being detected. This is important to factor into the design of vaccines: maybe we will need cytotoxic T cells and B cells to target different parts of the virus. Indeed, a study in macaques showed that a vaccine candidate targeting only the viral spike protein induced good, but not complete, protection.
Vaccines that do not induce full immunity are still important, of course, because they can lessen the severity or duration of infection. This is why designing vaccines is a complex process that requires a good understanding of immune responses.
We are still learning about COVID-19 and questions remain as to whether complete protection against it is even possible.
Issues still to be tackled
Another area of debate is whether some protection can arise from being infected with another coronavirus. There is some similarity between the version of coronavirus causing the current pandemic and others that cause a mild cold.
Some studies show a cross-reactivity, but others show none. Differences in these results may be down to how immune responses were analysed, or variations between people who could have had different prior exposures. Either way, such conflicting observations highlight the complexities involved.
Concerns have also been raised about the possibility of vaccines eliciting a response that could, at least in principle, produce antibodies that help the virus get into cells—a phenomenon known as antibody dependent enhancement.
The pressure to develop a vaccine is huge. The rush must not override the need for safety. There are other issues we must also tackle—not least, the manufacturing and fair distribution of anything that works. But right now, understanding the human immune response to this virus is our best hope and our greatest challenge.
Sheena Cruickshank and Daniel M Davis, The Conversation