The only antiviral drug currently used to treat SARS-CoV-2, the coronavirus that causes COVID-19, is remdesivir, but administering it is invasive and challenging. Scientists at The University of Texas at Austin are hoping to change that by using their novel thin-film-freezing technology to deliver remdesivir through dry powder inhalation, potentially making treatment more potent, easier to administer and more broadly available.
A team of researchers in UT Austin’s Division of Molecular Pharmaceutics and Drug Delivery, led by Robert O. (Bill) Williams III, has investigated varying methods of drug delivery to repurpose existing drugs into more efficacious forms. Earlier this year, the team focused on niclosamide, confirmed to exhibit antiviral efficacy in COVID-19 infected cells. Since then, remdesivir has emerged as the only available antiviral treatment for coronavirus.
Remdesivir is authorized for emergency use in adult and pediatric patients hospitalized with severe disease. Originally developed to treat the Ebola virus disease, remdesivir has shown promising results treating COVID-19 in the human airway epithelial cells. However, limited effective delivery methods have hindered efforts to provide widespread treatment to a broad range of patients exhibiting life-threatening symptoms.
“Unfortunately, remdesivir is not suitable for oral delivery since the drug is mostly metabolized by the body,” Williams said. “Intramuscular injection also faces challenges, since release rates from the muscles can vary widely.”
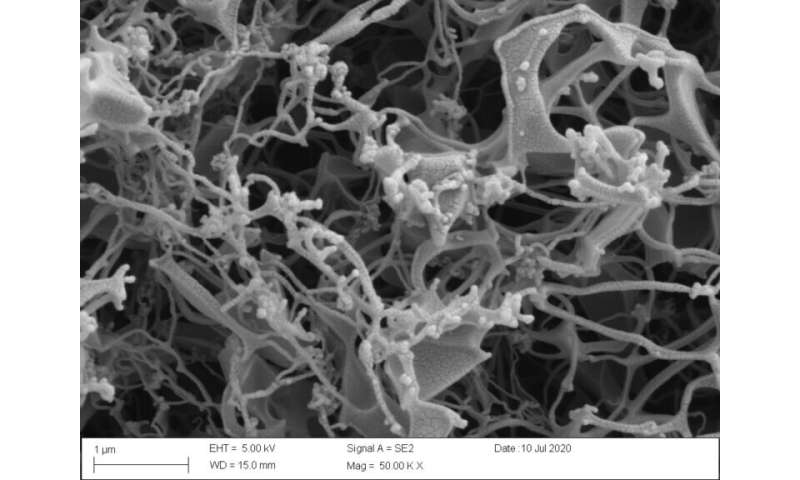
To provide remdesivir for other patients beyond the most severely ill, more convenient and accessible dosage forms for different routes of administration must be quickly developed and tested so patients have more options to get treated. One way to overcome the poor absorption rates of remdesivir is to deliver it directly to the infection site. The research team, which includes Sawittree Sahakijpijarn, Chaeho Moon and John J. Koleng, has developed inhaled forms of remdesivir for protecting and treating the respiratory mode of infection, including an amorphous brittle matrix powder made by thin-film freezing. Not only would this delivery method allow for wider distribution of an essential antiviral in the fight against COVID-19, it could also make remdesivir more effective.
“If patients can avoid a hospital visit to begin remdesivir treatment, it can lessen the current strains on our health system, lower cost and provide fewer points of contact with those who are still contagious,” Williams said. “More widely available early stage intervention methods could significantly lesson symptoms before they become potentially life-threatening, providing more hospital beds and ventilators to those who need them the most.”
TFF Pharmaceuticals Inc. has acquired the patents regarding thin-film freezing and inhalation. The UT researchers’ findings were recently published as a preprint in bioRxiv. Upon final study results, the team will submit its full findings for peer review and publication.
Nick Nobel, University of Texas at Austin

