We may not think about it often, but our gut is home to a complex ecosystem of microorganisms that play a critical role in how we function. The system is delicate—one small change can cause a major shift in the microbiome, resulting in serious consequences. When a person takes an antibiotic, it can wipe out multiple bacterial species and throw this delicate balance off-kilter. Clostridioides difficile is a common pathogen that colonizes a disrupted gut microbiota. Fecal microbiota transplantation (FMT), in which stool from a healthy donor is transplanted into the colon of a recipient, is a successful treatment for recurrent C. difficile infection (rCDI). In a recently published study, investigators from Brigham and Women’s Hospital explore how the dynamics of bacterial species may influence the success of FMT in treating rCDI. In Nature Communications, the team presents an algorithm to design personalized probiotic cocktails for patients with unhealthy gut microbiomes due to rCDI.
“Designing a probiotic cocktail is challenging,” said Yang-Yu Liu, Ph.D., an assistant professor in the Department of Medicine at the Brigham. “All of the species in the cocktail interact within a complicated network. When we look at one species that directly inhibits the growth of C. difficile, we must also make sure that it does not indirectly promote growth of C. difficile through interactions with other species in the cocktail.”
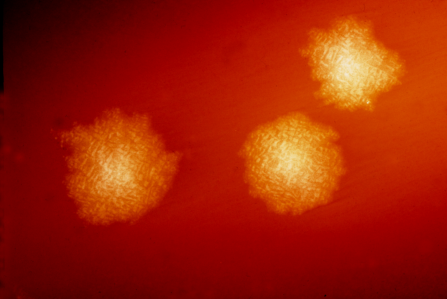
C. difficile is transmitted through the fecal-oral route—poor hygiene or the contamination of food or water supply—and is found all over the world. Although C. difficile will not typically colonize a healthy colon, it can grow unchecked in a gut that has been disrupted due to antibiotics. rCDI is not responsive to standard antibiotics and therefore can recur in patients, increasing the risk each time. FMT has been shown to cure about 80 percent of rCDI cases that did not respond to antibiotics.
The researchers began by modeling a microbial community and simulating the FMT process of treating rCDI. Next, they estimated how effective FMT would be at restoring the recipient’s healthy gut microbiota. The team then analyzed real-world data from a mouse model and from human patients to validate the modeling.
The theoretical model helped the team predict what factors determine the efficacy of FMT. They learned that FMT efficacy decreases as the species diversity of the infected person’s gut microbiome increases. The team also developed an optimization algorithm to design a personalized probiotic cocktail to help individuals with rCDI. The algorithm is based on ecological theory that designs a cocktail with the minimum number of bacterial species, while keeping the complicated ecological network of the species in mind. The personalized probiotic cocktails contain species that are effective inhibitors of C. difficile and can be administered to patients with rCDI in order to restore their gut microbiota.
“We now have an ecological understanding of FMT—why it works and why it sometimes fails for rCDI,” said Liu. “We can move forward to better understand the efficacy of FMT and how we can use it to treat other diseases associated with disrupted microbiota, such as IBD, autism and obesity.”
Brigham and Women’s Hospital

