Autism spectrum disorder (ASD) is rarely diagnosed until symptoms arise, often well into childhood. Evidence however, is mounting that developmental abnormalities likely emerge in the brain long before then: early identification of babies at risk for ASD could allow for interventions that would improve their developmental outcomes.
Researchers at the University of California, Los Angeles, have found evidence of signature brain activity in infants that predicted ASD symptoms later at 18 months old. The work, led by Shafali Jeste, MD, at UCLA appears in Biological Psychiatry: Cognitive Neuroscience and Neuroimaging.
“Early identification and intervention is key to getting better outcomes for children with neurodevelopmental disorders,” said Cameron Carter, MD, Editor of Biological Psychiatry: Cognitive Neuroscience and Neuroimaging. “This study suggests that relatively low-cost diagnostic tools such as EEG may, in the not-too-distant future, help us to do a better job by identifying atypical brain development in infancy, when interventions may be even more impactful than when offered to toddlers and young children.”
The researchers used electroencephalography (EEG), a non-invasive technique to measure electrical brain activity from outside the head and tracked neural activity in the so-called alpha range. Alpha-range activity is associated with long-range connections in the brain. The group then used an approach that allowed them to integrate data from across the brain.
First author Abigail Dickinson, Ph.D., said, “One crucial aspect of brain development is the change in patterns of brain activity. We wanted to know if measures of neural activity could detect atypical brain development in ASD during early infancy.”
Dr. Dickinson and the team performed EEG measurements in 65 3-month-old infants; 29 with low familial risk of ASD and 36 at high risk, with an affected older sibling.
When the children were 18-months-old, they were assessed for ASD by a trained clinician.
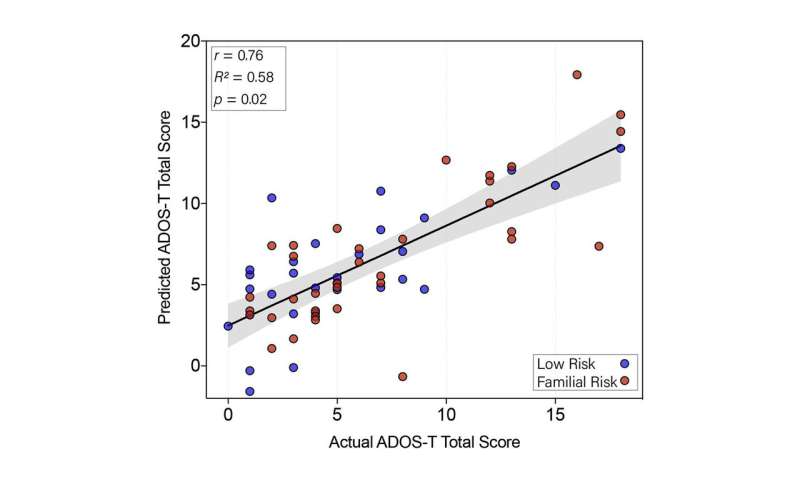
The researchers used computer modeling to predict symptom outcomes at 18 months based on the babies’ neural activity in infancy. The model’s predictions correlated with the actual symptoms measured in the toddlers. The model was not able to predict verbal or non-verbal congitive scores in the toddlers—suggesting that the brain connectivity pattern may be a specific marker of ASD.
In infants that later showed higher ASD symptoms, researchers saw decreased connectivity between frontal regions. The infants also showed increased connections across temporo-parietal areas in the right hemisphere, which are associated with social information processing.
“These findings improve our understanding of the neural differences that precede autism and show which brain regions reveal the earliest signs of disruption,” Dr. Dickinson said. The findings bolster the idea that disrupted brain connectivity is a root cause of ASD, not a consequence.
The authors suggest that the low cost, wide availability and low risk of EEG make it a good screening tool to identify babies at higher risk of developing ASD or those with “borderline” symptoms, so that they get early intervention. “Mapping patterns of activity associated with autism could ultimately help identify infants who show early signs of neural risk,” Dr. Dickinson added.
Elsevier

