As countries around the world race to develop a vaccine for SARS-CoV-2, the virus responsible for COVID-19, researchers are working to understand exactly how it causes the myriad of symptoms that seem to linger long after active viral infection. In a study published in scientific journal PNAS, researchers led by Osaka University identified an effective treatment for the deadly over-activation of the inflammatory response seen in many severe COVID-19 patients.
Cytokines are a group of small proteins that can either enhance or inhibit our body’s immune response to infection, trauma, and diseases such as cancer. One of their main roles is to stimulate inflammation, which initiates the healing process. The problem is, overstimulation of the inflammatory response has an array of harmful complications, ranging from asthma to severe autoimmune diseases. One such complication, called cytokine release syndrome (CRS), is seen in patients suffering a hyperimmune response to microbial infection or trauma and can lead to multiple organ failure and even death.
“Despite knowing which cytokines are involved, there is still no specific immunotherapy for CRS and treatment is limited to supportive care,” says study lead author Sujin Kang. “To better understand the molecular mechanisms of CRS pathogenesis, we first studied the cytokine profiles of 91 patients diagnosed with CRS associated with bacterial sepsis, acute respiratory distress syndrome, or burns.”
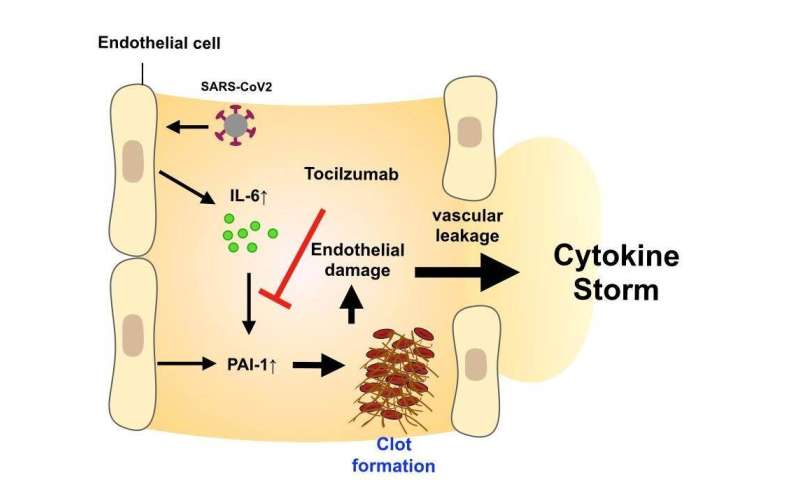
Strikingly, patients from all three groups had elevated levels of proinflammatory cytokines IL-6, IL-8, IL-10, and MCP-10, as well as a protein called PAI-1, which causes small blood clots in vessels throughout the body, including the lungs. Importantly, increased PAI-1 levels are associated with more severe cases of pneumonia, a common cause of death among COVID-19 patients.
Because IL-6 was positively associated with the levels of the other cytokines and PAI-1, the researchers concluded that IL-6 signaling is crucial for the development of CRS following infection or trauma, and may play a role in the pathogenesis of COVID-19.
“Examination of cytokine profiles in severe COVID-19 patients revealed an increase in IL-6 early in the disease process, causing release of PAI-1 from blood vessels,” says study senior author Tadamitsu Kishimoto. “Interestingly, PAI-1 levels were significantly higher in COVID-19 patients with severe respiratory impediment.”
Most significantly though, when severe COVID-19 patients were treated with a human monoclonal antibody-based drug called Actemra, which blocks IL-6 signaling, PAI-1 levels rapidly declined and severe disease symptoms were alleviated. IL-6 signaling blockade could therefore prove useful for the treatment of both CRS and the severe respiratory complications of COVID-19.
Osaka University

