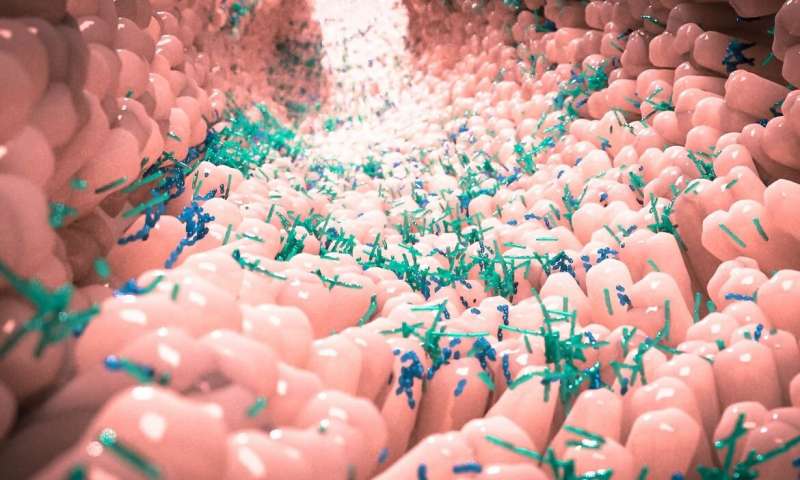
During pregnancy in mice, the billions of bacteria and other microbes that live in a mother’s intestines regulate key metabolites, small molecules that are important for healthy fetal brain development, UCLA biologists report Sept. 23 in the journal Nature.
While the maternal gut microbiota has been associated with abnormalities in the brain function and behavior of offspring—often in response to factors like infection, a high-fat diet or stress during pregnancy—scientists had not known until now whether it influenced brain development during critical prenatal periods and in the absence of such environmental challenges.
To test the impact the gut microbiata has on the metabolites and other biochemicals that circulate in maternal blood and nurture the rapidly developing fetal brain, the researchers raised mice that were treated with antibiotics to kill gut bacteria, as well as mice that were bred microbe-free in a laboratory.
“Depleting the maternal gut microbiota, using both methods, similarly disrupted fetal brain development,” said the study’s lead author, Helen Vuong, a postdoctoral scholar in laboratory of UCLA’s Elaine Hsiao.
Depleting the maternal gut microbiota altered which genes were turned on in the brains of developing offspring, including many genes involved in forming new axons within neurons, Vuong said. Axons are tiny fibers that link brain cells and enable them to communicate.
In particular, axons that connect the brain’s thalamus to its cortex were reduced in number and in length, the researchers found.
“These axons are particularly important for the ability to sense the environment,” Vuong said. “Consistent with this, offspring from mothers lacking a gut microbiota had impairments in particular sensory behaviors.”
The findings indicate that the maternal gut microbiota can promote healthy fetal brain development by regulating metabolites that enter the fetal brain itself, Vuong said.
“When we measured the types and levels of molecules in the maternal blood, fetal blood and fetal brain, we found that particular metabolites were commonly decreased or missing when the mother was lacking a gut microbiota during pregnancy,” she said.
The biologists then grew neurons in the presence of these key metabolites. They also introduced these metabolites into the microbiata-depleted pregnant mice.
“When we grew neurons in the presence of these metabolites, they developed longer axons and greater numbers of axons,” Vuong said. “And when we supplemented the pregnant mice with key metabolites that were decreased or missing when the microbiata was depleted, levels of those metabolites were restored in the fetal brain and the impairments in axon development and in offspring behavior were prevented.
“The gut microbiota has the incredible capability to regulate many biochemicals not only in the pregnant mother but also in the developing fetus and fetal brains,” Vuong said. “Our findings also pinpoint select metabolites that promote axon growth.”
The results suggest that interactions between the microbiota and nervous system begin prenatally through the influence of the maternal gut microbiota on the fetal brain, at least in mice.
The applicability of the findings to humans is still unclear, said the study’s senior author, Elaine Hsiao, a UCLA associate professor of integrative biology and physiology, and of microbiology, immunology and molecular genetics in the UCLA College.
“We don’t know whether and how the findings may apply to humans,” said Hsiao, who is also an associate professor of digestive diseases at the David Geffen School of Medicine at UCLA. “However, there are many neurodevelopmental disorders that are believed to be caused by both genetic and environmental risk factors experienced during pregnancy. Our study suggests that maternal gut microbiota during pregnancy should also be considered and further studied as a factor that could potentially influence not only the health of the mother but the health of the developing offspring as well.”
Hsiao, Vuong and colleagues reported in 2019 that serotonin and drugs that target serotonin, such as antidepressants, can have a major effect on the gut’s microbiota. In 2018, Hsiao and her team established a causal link between seizure susceptibility and gut microbiota and identified specific gut bacteria that play an essential role in the anti-seizure effects of the ketogenic diet.
Stuart Wolpert, University of California, Los Angeles