New research from north-west England published in Anaesthesia (a journal of the Association of Anaesthetists) shows that during the first wave of COVID-19, the proportion of caesarean section deliveries carried out under general anaesthesia approximately halved, from 7.7% to 3.7%. This lower rate of general anaesthesia (also 3.7%) was also found among the small number of women having caesarean sections who had tested positive for COVID-19.
“At the onset of the global pandemic of COVID-19 (SARS-CoV-2), guidelines recommended using regional anaesthesia for caesarean section in preference to general anaesthesia, in order to reduce the risk of SARS-CoV-2 infection in healthcare workers,” say the authors, who include Dr. Kailash Bhatia, Saint Mary’s Hospital (part of Manchester University NHS Foundation Trust), and The University of Manchester; Dr. Malachy Columb, Wythenshawe Hospital (part of Manchester University NHS Foundation Trust), UK, and colleagues. “Anaesthetic decision-making, recommendations from these anaesthetic guidelines, and the regular presence of an on-site anaesthetic consultant in the delivery suite throughout the first wave could be among the key factors that influenced this decline.”
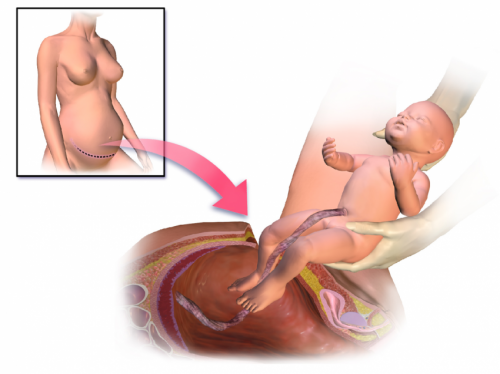
National figures from the UK show that almost 170,000 caesarean sections were carried out in 2016-17 and approximately 8.75% (around 15,000) were performed under a general anaesthetic. In this new study, the authors explored whether general anaesthesia rates for women having caesarean sections changed during the peak of the pandemic across six maternity units in the north-west of England.
They analysed data for 2480 caesarean sections across these six maternity units from 1 April to 1 July 2020 and compared this information with data from 2555 caesarean sections performed at the same hospitals over a similar period in 2019.
The data revealed a significant reduction (7.7% to 3.7%) in general anaesthetic rates for women having caesarean sections, with analysis showing that a woman having a caesarean section birth during this period in 2020 was half as likely to have it under general anaesthetic than a woman having the procedure in 2019. The authors also found that the rate of conversion from local to general anaesthesia (done for emergency reasons during the procedure) also halved from 1.7% to 0.8% from 2019 to 2020.
Their analysis found no differences between 2019 and 2020 for the obstetric indications for caesarean sections. However, the overall rate of caesarean sections in all births in these samples increased from 28.3% in 2019 to 29.7% in 2020.
Dr. Bhatia said: “It has been known for a long time that regional anaesthesia—i.e. a spinal epidural—is safer than general anaesthesia for caesarean sections. It has other benefits which include better pain relief; both partners being able to share in the birth experience in theatre during the procedure and earlier skin to skin contact with the baby.
“However, during the current COVID-19 pandemic, there are additional concerns that if a woman who has the virus is given a general anaesthetic, she could develop more serious respiratory problems than if she had a regional anaesthetic, and it is therefore even more important that general anaesthetics are avoided where possible. Women in labour may require a caesarean section before the team caring for them know whether she has COVID-19 or not, and therefore in these women, it is also important to avoid general anaesthesia if possible.
“General anaesthesia not only puts the woman having the caesarean section at risk of respiratory problems, but also anaesthetic staff and other healthcare workers in theatre, as tracheal intubation is an aerosol-generating procedure which poses a high risk of viral transmission from a suspected or confirmed case. It is therefore not surprising that anaesthetists were keen to avoid general anaesthesia—unless regarded as essential—in order to ensure the safest possible care for patients, and a safe working environment for staff.”
In the paper, the authors also stress that general anaesthesia was still used when required in emergency situations, termed category one caesarean sections (which represent around one in six of all caesarean sections in the UK), and include situations such as fetal distress that require immediate action. In this study, the rate of general anaesthesia in the 2020 group was 12% among these category one caesarean sections, well above the overall 2020 group average of 3.7%, but also well below the rate of 25% rate for category one caesarean sections seen in the 2019 group.
Also of note was that anaesthetic staffing changed during the pandemic. On-site out-of-hours anaesthetic consultant support systems were established in 80% of the hospitals analysed. “During the first wave of the COVID-19 pandemic, most of the maternity units we studied benefitted from the presence of more experienced and skilled personnel in the delivery suite, leading to improved on-site immediate and local supervision. This possibly contributed to the high regional anaesthesia rates and lower regional to general anaesthesia conversion rates compared to the pre-COVID group,” explain the authors.
They add: “Personal protective equipment (PPE) recommendations were different for women needing regional anaesthesia and at low risk of a conversion to a general anaesthesia (droplet precautions) compared with those having general anaesthesia from the commencement of caesarean section or those at high risk of conversion (airborne precautions). Donning of PPE for general anaesthesia takes time, which could theoretically result in adverse fetal outcomes in urgent/emergency caesarean sections. It is possible that this factor may have contributed to decision-making by anaesthetists.”
The authors also discuss specific findings on women who tested positive for COVID-19. A total of 76 of 2480 (3%) of women tested positive in this study and the caesarean section rate for COVID-19 positive women was 36% (27 women), higher than the 29.7% reported for the 2020 group overall, but much lower than reported in other studies. Just one of these 27 women had general anaesthesia, the same proportion (3.7%) as in the 2020 group overall.
However the authors caution: “We would not want to draw any specific conclusions as we do not have the details for these women. We do not know the number of women who were swabbed for COVID-19 across hospitals regionally, and cannot therefore estimate the incidence of COVID-19 in these hospitals. We would like to highlight the fact that our dataset has one of the lowest caesarean section rates reported for COVID-19 positive pregnant women.”
They conclude: “Overall, we conclude that the general anaesthesia rate for women having caesarean sections declined significantly during the peak of the COVID-19 pandemic. Anaesthetic decision-making recommendations from anaesthetic guidelines and presence of an on-site anaesthetic consultant in the delivery suite could be among the key factors that potentially influenced this decline.”
“One of the important questions this study raises is: why do trainees seemingly choose general anaesthesia more frequently when they are working solo?” adds Dr. Tim Meek of the Association of Anaesthetists, a consultant anaesthetist based at James Cook University Hospital, Middlesbrough, UK. “Possible explanations include lack of confidence in their regional anaesthesia skills, a perception that general anaesthesia is always quicker and, perhaps most importantly, a disproportionate focus on target decision to delivery times as the key marker of success. We should now aim to identify what enables consultants to provide regional anaesthesia confidently and focus on equipping trainees with those tools to the benefit of the women and babies we all care for.”
AAGBI

