Findings from a national study published today in the Journal of the American Medical Association (JAMA) “do not support” the use of hydroxychloroquine for the treatment of adult patients hospitalized with COVID-19.
The Outcomes Related to COVID-19 treated with Hydroxychloroquine among In-patients with symptomatic Disease (ORCHID) study found that, when compared to inactive placebo, hydroxychloroquine did not significantly improve clinical outcomes of patients hospitalized for respiratory illness related to COVID-19.
The study, which was funded by the National Heart, Lung, and Blood Institute (NHLBI) of the National Institutes of Health, was conducted at 34 hospitals in the Prevention and Early Treatment of Acute Lung Injury (PETAL) Clinical Trials Network.
“Hydroxychloroquine became a very commonly used medication for COVID-19 in the spring of 2020 without strong evidence that it would be beneficial,” said the study’s lead investigator, Wesley H. Self, MD, MPH, an emergency medicine physician and vice president for Clinical Research Networks and Strategy at Vanderbilt University Medical Center.
“Therefore, we conducted a clinical trial with the strongest methods possible to provide high quality information on whether hospitalized patients with COVID-19 should be treated with hydroxychloroquine,” Self said. “Combined with other studies that showed similar findings, we believe this trial provides compelling data for clinicians to stop using hydroxychloroquine for hospitalized adults with COVID-19.”
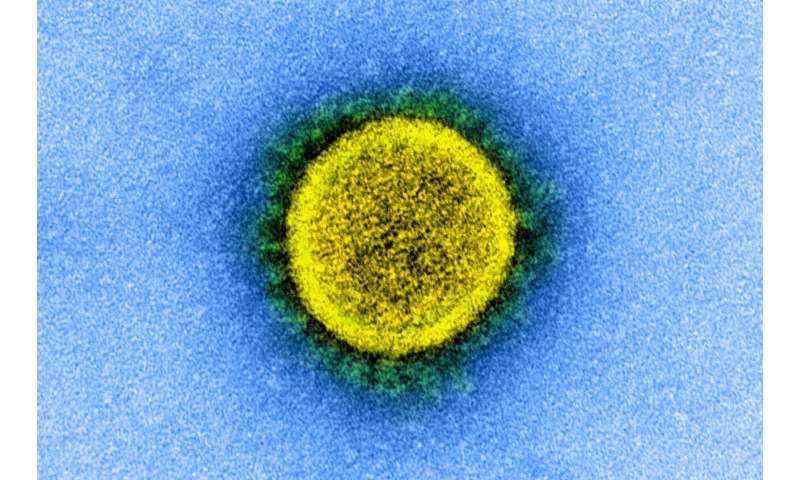
Some laboratory studies suggested hydroxychloroquine can inhibit replication of SARS-CoV-2, the virus that causes COVID-19. Observational studies early in the COVID-19 pandemic suggested that the drug may have beneficial effects for patients with COVID-19, which sparked great enthusiasm for hydroxychloroquine as a potential treatment.
However, clinical trials, which are considered the highest quality research studies for understanding the effect of a drug in patients, have failed to show beneficial effects of hydroxychloroquine for patients with COVID-19, Self said.
Between April and June 2020, 479 patients hospitalized for respiratory illness from COVID-19 were enrolled in the ORCHID study, a blinded, placebo-controlled randomized clinical trial.
Patients who were acutely ill and hospitalized with COVID-19 were treated with 10 doses of hydroxychloroquine or placebo over five days. The patient’s clinical status, including hospital discharge, oxygen use, mechanical ventilator use and death, was followed for a month after the medication was started.
The study showed no evidence that hydroxychloroquine prevented death or helped patients recover from COVID-19 more quickly. One month after starting the study, 10.4% of patients treated with hydroxychloroquine and 10.6% of patients treated with placebo had died.
In June the NHLBI halted the study after determining that hydroxychloroquine was not likely to be of benefit to hospitalized patients with COVID-19.
“Our diverse teams of clinicians and research staff worked nimbly under extremely difficult circumstances to accomplish what the NIH and the PETAL Network do best: ‘gold standard’ studies of important questions for patients suffering from life-threatening conditions,” said Samuel M. Brown, MD, MS, a critical care physician at Intermountain Healthcare and PETAL Network investigator who helped lead the trial.
“While we hoped that hydroxychloroquine would help, even this clearly negative result is critical as we work together to find effective treatments for COVID-19,” Brown said.
“Having a rigorously designed clinical trial that captured patient-centered, clinically meaningful outcomes was critical to reaching the unequivocal conclusions about the use of hydroxychloroquine in COVID-19,” said James P. Kiley, Ph.D., director, Division of Lung Diseases at NHLBI.
“ORCHID shows that hydroxychloroquine does not improve clinical outcomes in hospitalized COVID-19 patients,” Kiley said. “We hope this clear result will help practitioners make informed treatment decisions and researchers continue their efforts pursuing other possible safe and effective treatments for patients suffering with this disease.”
Vanderbilt University Medical Center

