Autoinflammatory syndromes are often the result of genetic mutations that ultimately compromise neutrophils, macrophages and other cells of the innate immune system. Rather than showering sufferers with broad immunosuppressives, a more satisfactory response can frequently be obtained using select anti-inflammatory drugs like anti-TNF or anti-IL-1β. A similar inappropriate innate activation is now commonly observed in susceptible individuals who have progressed to acute respiratory distress after SARS-CoV-2 infection. In trying to fight back against a pathogen surveillance system that has gone haywire, many are now asking how we might do better.
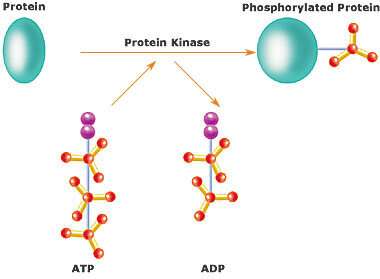
One way to try to finesse a stubborn immune system is to unplug specific subcellular signaling pathways using kinase inhibitors. Small-molecule inhibitors of various immune-specific kinases, including JAKs, IRAK4, RIPKs, BTK, SYK and TPL2, are now in the clinic. A paper recently published in Nature Reviews summarizes the current state of the art in therapeutic kinase control of immunity and inflammation. Documenting this rapidly proliferating field is no small task, as it is estimated that up to one-third of our proteome is phosphorylated to significant effect in numerous places. The above-mentioned immune-related TNF superfamily itself contains 19 members acting on some 29 receptors, while the IL-1 receptor family has 10 members.
While host immunity is usually divided into strictly innate and strictly adaptive immune systems, the reality is that things are not that simple. In a nutshell, the innate system typically reacts quickly and non-specifically to pathogens, whereas the adaptive system generates a slower, more specific response culminating in a long-lived immunological memory. The transition of power from the former to the latter involves a tricky hand-off mediated by numerous cytokines such as the interferons and interleukins.
One way to better visualize things here is to consider an infection of the body to be analogous to what happens when electrical power is suddenly cut off to a hospital. Since many legacy life support systems and other critical instruments might reboot into a less than adequately defined state, sophisticated uninterruptible power systems (UPSs) stand by to prevent that from happening. When a glitch is detected, the UPS must react within one-60th of a second (or one-50th in Europe) to seamlessly deliver inverter power from the reserve battery bank. But like the innate immune system, the batteries are really just a temporary stop gap until the heavy hitters, the dedicated diesel generators sitting out back, can be spooled up to take over. Once online, the generators can adapt to further fluctuations in power and maintain continuous long-term power until health is restored.
The problem in all this is that one cannot just flip a big switch and instantly change from one service to another. The new source must be synchronized with some precision to the old source. In other words, the phases on each line must be in synch or else their peaks and valleys will be shoved together in an unpredictable fashion with potentially disastrous results. Furthermore, just like in a vehicle’s ignition system, the main solenoid switches themselves need other switches to turn them on, and those, in turn, often require even tinier switches. In the immune system, many of the low-level switches are kinases. These are basically the minimum biological bits that can be readily set or erased to control the state of the system.
The JAK family of kinases (Janus kinases) includes JAK1, JAK2, JAK3 and a non-receptor tyrosine-protein kinase called TYK2. These kinases transduce signaling of cytokines like IL-2R, IL-4R, IL-5R, IL-6R, IL-13R and type I interferons to dedicated combinations of the six STAT family members, ultimately leading to STAT dimerization and translocation to the nucleus to regulate genes. Although JAK inhibitors (JAKi) have been deployed for autoimmune diseases such as rheumatoid arthritis and asthma, their use for more pressing matters, like COVID-19, are now under consideration.
Since viruses take over a large number of host kinases at distinct steps of their life cycle, kinases represent attractive targets for broad-spectrum therapy. Different JAKi, like baricitinib for example, can impair SARS-CoV-2 endocytosis and the early stages of virus spread, while at the same time inhibiting emergence of a cytokine storm. This so-called HiJAKing therapy often looks good on paper, but special care may be needed in practice, as some folks might take issue. For example, JAKi administration is known to result in an increased risk of varicella zoster reactivation in rheumatoid arthritis patients.
In another recent Nature paper, Pairo-Castineira et. al., conducted genome-wide and transcriptome-wide association studies on critical care COVID-19 patients. They found evidence for causal links with several immune-related proteins, including high expression of TYK2, low expression of IFNAR2, and the monocyte/macrophage chemotactic receptor CCR2 to severe COVID-19. While many critical COVID-19 patients show clear evidence of cytokine storm, other researchers have noted fundamental differences between COVID cytokine release and that typically seen in patients experiencing autoimmune inflammation or in those receiving immunotherapies like CAR-T cell therapy. In the COVID-style “cytokine breeze,” there is often a lower cytokine concentration, but the levels are maintained over a longer period of time.
None of this has escaped the attention of Big Pharma. Other classes of tyrosine kinase inhibitors, like the BTK inhibitor ibrutinib, are also being tested for their ability to interfere with cytokine release syndrome, and protect against severe lung injury in COVID patients. Contract-for-hire drug discovery services are now a critical mainstay to help rapidly identify potential targets for addressing COVID. Phosphoproteomics analysis of SARS-CoV-2-infected cells is also now being used to uncover the global phosphorylation landscape of SARSCoV-2 Infection. This effort represents nothing short of divining the total effect of SARS on the phosphorylation status of the cell. In particular, it was found that SARS infection promoted casein kinase II (CK2) and p38 MAPK activation, and stimulated CK2-containing filopodial protrusions possessing budding viral particles.
Of pressing interest in all things COVID is not necessarily who is susceptible to infection, but rather, who is going to need to be put on a vent? In the timeless question of nature vs. nurture, susceptibility to SARS seemingly falls squarely within the nature box. For example, a coding variant in the TYK2 gene, as alluded to above, protects from multiple autoimmune diseases and has even been used to enable rational drug design. This particular substitution swaps in an alanine residue for a proline at location 1104 in the catalytic domain to prevent receptor-mediated activation. The drug, BMS-986165, allosterically blocks TYK2 activation via a mechanism similar to that of the coding variant.
Other studies have shown that variants in the TMEM41B gene, which are common in East Asians, may explain the disproportionate severity of COVID-19 illness among some populations in the United States and elsewhere. Much the same, multiple heparan sulfate biosynthetic genes (B3GALT6, B3GAT3, B4GALT7, EXT1, EXT2, EXTL3, FAM20B, NDST1, SLC35B2, UGDH, XYLT2) were also identified in genetic screens that are consistent with reports showing SARS-CoV-2 requires both ACE2 and cellular heparan sulfate for efficient infection.
As we reported last week, the success of vaccines against SARS depends on many factors, not least of which is the kind of immunity-confering antibodies clinicians want to encourage. We can offer that only fools would put all their eggs in the vaccine basket. While the FDA has finally divulged what it thinks might be the ingredients list for the newly released Pfizer mRNA vaccine, the actual sequence of the business end is still shrouded in secrecy. To be sure, the vaccine’s mRNA can’t be quite the same stuff that we normally make in our bodies. Instead, modified nucleosides are likely substituted to defeat host defenses ready to chop up any offending RNA.
In the void of actual sequence knowledge, the predictably illuminating forces of conspiracy have begun to emerge. For example, some have noted that the vaccine might not just target the spike protein, but also any host proteins that happen to resemble it. One example might be the HERV (human endogenous retrovirus) protein Syncytin-1, which helps trophoblasts fuse to form the placenta. For now, the degree of sequence overlap and structural homology remains to be seen.
While the question of who should get vaccines or costly treatments for SARS first has been highly politicized in recent times, we can only hope that clear heads will prevail. When the New York Times is quoting medical ethics professors who claim that certain people must be de-emphasized for vaccine priority based on their skin color, it might be time to look for better options.
John Hewitt , Medical Xpress

