Recently there have been significant advances on several fronts in the ongoing war against cancer of the alimentary tract. Now, Japanese researchers report the development of another weapon: Linked Color Imaging (LCI), a novel endoscopic technique that improves detection of cancer by viewing the upper digestive tract mucosa under illumination that combines specific wavelengths of light to intensify subtle color variations indicative of neoplastic change.
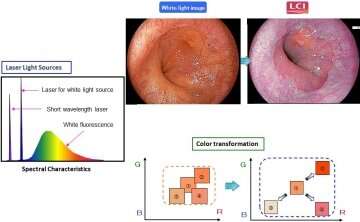
Upper gastrointestinal (GI) endoscopy is routinely performed to detect tumorous changes or neoplasia in the pharynx, esophagus, and stomach and is conventionally done under White Light Imaging (WLI). Using the innovative LASEREO system developed by the Fujifilm Corporation, LCI technology balances white light with narrow-band short wavelength light in a specific ratio that deepens and enhances the contrast of red and white hues, thus intensifying nuances of mucosal transformation.
Though earlier studies have described the role of LCI in histological diagnosis of upper GI tract tumors, the research team felt the need for a large-scale, broad-based comparative study to assess its efficacy in neoplasm detection. “Our research was conducted in 19 hospitals across Japan involving 1502 patients with known past or current gastrointestinal cancer, representing a high-risk population” explains Dr. Shoko Ono, lead author. “Patients underwent upper GI endoscopy under both WLI and LCI protocols wherein they were grouped according to which modality was performed first. Ingeniously, our study design ensured diagnostic accuracy; not only did each modality serve as a backup and crosscheck on the other, this was further followed by histopathological confirmation.”
Dr. Kenro Kawada, co-lead author, describes the results. “With LCI, lesions were detected in 8% of the patients but the detection rate was only 4.8% with WLI. Conversely, with WLI 3.5% of patients had a lesion overlooked but this rate was only 0.67% with LCI. This shows a clear superiority of LCI over conventionally illuminated endoscopic screening for discerning mucosal changes related to upper GIT neoplasia as it detected neoplasia 1.67 times more frequently.”
Professor Mototsugu Kato, senior and corresponding author, explains the implications of their research. “Combined with previous studies that show the efficacy of LCI in detecting large intestinal neoplasia, our findings make a strong case for wider adoption of this modality in surveillance of the entire endoscopically accessible digestive tract. However, we need further research to confirm its efficacy in the hands of general clinicians for upper GI screening of an average population.”
Tokyo Medical and Dental University

