Modern immunotherapeutic anti-cancer drugs support a natural mechanism of the immune system to inhibit the growth of cancer cells. They dock onto a specific receptor of the killer cell and prevent it from being switched off by the cancer cells. This is a complex molecular process, which is known but has not yet been fully understood. In a molecular dynamics study conducted by the group led by medical information scientist Wolfgang Schreiner and gynecologists Heinz Kölbl and Georg Pfeiler from MedUni Vienna, working with biosimulation expert Chris Oostenbrink from the University of Natural Resources and Applied Life Sciences (Boku) Vienna, has now, for the first time, analyzed this mechanism for the drugs nivolumab and pembrolizumab. It was found that tiny molecular motions are of key significance. The study has been published in the leading journal Cancers.
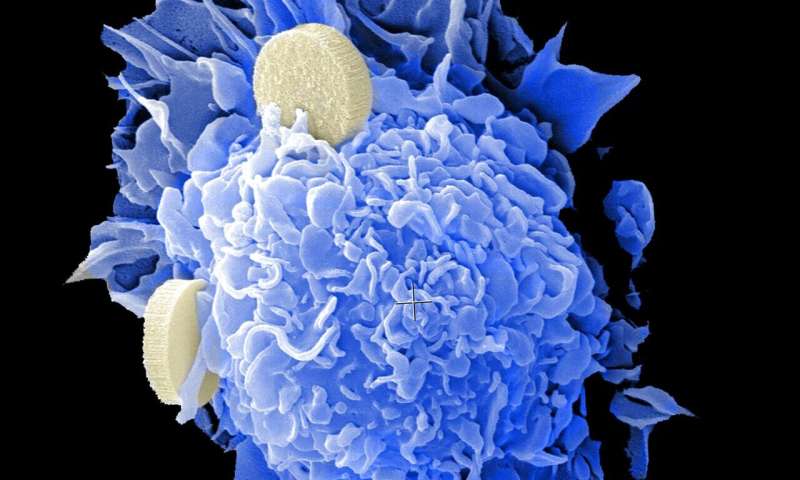
The human immune system protects the body against bacteria, viruses and damaged cells, such as cancer cells. Specialized immune cells, such as natural killer cells (NK cells), work together to identify and eliminate these threats. Sometimes these killer cells inadvertently target healthy cells, and this can result in severe autoimmune reactions. If this happens, the immune system deploys a safeguard measure, so-called “programmed cell death” (apoptosis). This is triggered when the endogenous surface molecule PD-L1 binds to the receptor expressed on the killer cell, the PD- molecule. In this process, the (immuno-checkpoint) receptor acts like an emergency off switch. If cells are attacked in error, they produce PD-L1 molecules and reach towards the killer cells, thus killing them. Cancer cells are also able to express PD-L1 and these bind to the checkpoint, thereby causing the killer cells to die and allowing the tumor to grow.
This is exactly where modern immunotherapeutic anti-cancer drugs (checkpoint inhibitors) come in. They resemble the surface molecule PD-L1 and bind to the PD-1 receptor, but the triggered mechanism is different, as the killer cells are not sent into cell death. Although the checkpoints are blocked, they are not activated. Cancer cells are no longer able to bind to the blocked receptors and the killer cells retain their ability to destroy cancer cells. Immunotherapy exploits this phenomenon, even though it was hitherto not fully understood exactly how the binding occurred without a switching process.
Wolfgang Schreiner from the Center for Medical Statistics, Informatics and Intelligent Systems at MedUni Vienna’s Institute of Biosimulation and Bioinformatics, gynecologists Georg Pfeiler and Heinz Kölbl, who is also Director of MedUni Vienna’s Department of Obstetrics and Gynecology, and Chris Oostenbrink from Boku Vienna, have now investigated the key differences between the natural PD-L1 and the drugs used for treating various cancers such as breast cancer, lung cancer and melanoma in a molecular dynamics model by means of computer simulation. The motions of individual atoms and their reciprocal influence were calculated and mathematically analyzed on the supercomputer belonging to Vienna Scientific Cluster (VSC). In this way it was possible to identify the smallest differences in the molecular motions between the natural molecule PD-L1 and those of the drugs.
Schreiner explains: “One can virtually make a precise mathematical assessment of the ‘facial expressions’ of the molecules in slow motion, up close and personal. It was found that some loops of the PD-1 molecule deform in a different way, depending on their binding partner.” These small differences would be directed inside the killer cell by the PD-1 molecule and produce the desired effect, namely that, although the drugs would bind to the receptor, they would not activate it like the natural surface molecule PD-L1.
What initially appears to be a slight difference is actually the basis for our continually growing understanding of cellular processes. The more we know about these, the more specific we can be in the development of checkpoint inhibitors. Research findings of this kind are highly promising, particularly in the area of gynecological oncology, says Pfeiler: “Of course, checkpoint inhibitors can only work if the corresponding surface molecules (PD-1, PDL-1) that are to be inhibited, are actually expressed. This therapy is then a good option for triple negative breast cancer, for example. Interestingly, to date, only the expression of PDL-1 has been observed pre-therapeutically but not the expression of PD-1. This raises manifold research questions in terms of precision medicine.”
Medical University of Vienna

