Tumors can be damaging to surrounding blood vessels and tissues even if they’re benign. If they’re malignant, they’re aggressive and sneaky, and often irrevocably damaging. In the latter case, early detection is key to treatment and recovery. But such detection can sometimes require advanced imaging technology, beyond what is available commercially today.
For instance, some tumors occur deep inside organs and tissues, covered by a mucosal layer, which makes it difficult for scientists to directly observe them with standard methods like endoscopy (which inserts a small camera into a patient’s body via a thin tube) or reach them during biopsies. In particular, gastrointestinal stromal tumors (GISTs)—typically found in the stomach and the small intestines—require demanding techniques that are very time-consuming and prolong the diagnosis. Now, to improve GIST diagnosis, Drs. Daiki Sato, Hiroaki Ikematsu, and Takeshi Kuwata from the National Cancer Center Hospital East in Japan, Dr. Hideo Yokota from the RIKEN Center for Advanced Photonics, Japan, and Drs. Toshihiro Takamatsu and Kohei Soga from Tokyo University of Science, Japan, led by Dr. Hiroshi Takemura, have developed a technology that uses near-infrared hyperspectral imaging (NIR-HSI) along with machine learning. Their findings are published in Nature’s Scientific Reports.
“This technique is a bit like X-rays, the idea is that you use electromagnetic radiation that can pass through the body to generate images of structures inside,” Dr. Takemura explains, “The difference is that X-rays are at 0.01-10 nm, but near-infrared is at around 800-2500 nm. At that wavelength, near-infrared radiation makes tissues seem transparent in images. And these wavelengths are less harmful to the patient than even visible rays.”
This should mean that scientists can safely investigate something that is hidden inside tissues, but until the study by Dr. Takemura and his colleagues, no one had attempted to use NIR-HSI on deep tumors like GISTs. Speaking of what got them to go down this line of investigation, Dr. Takemura pays homage to the late professor who began their journey: “This project has been possible only because of late Prof. Kazuhiro Kaneko, who broke the barriers between doctors and engineers and established this collaboration. We are following his wishes.”
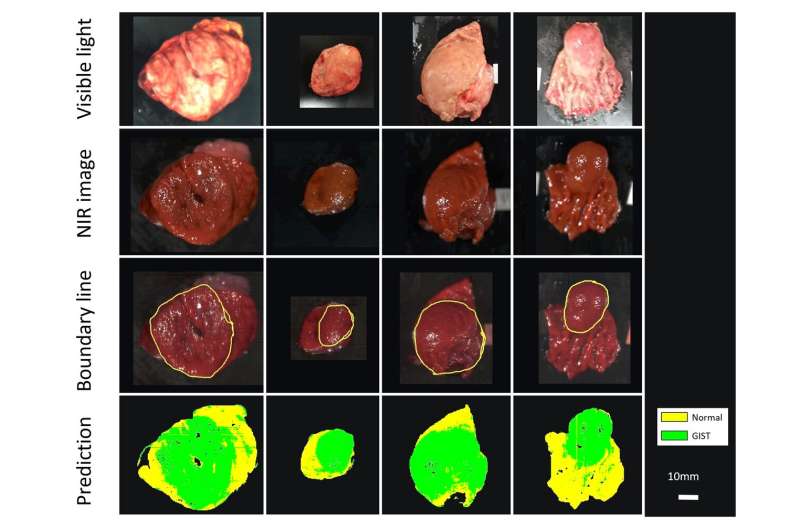
Dr. Takemura’s team performed imaging experiments on 12 patients with confirmed cases of GISTs, who had their tumors removed through surgery. The scientists imaged the excised tissues using NIR-HSI, and then had a pathologist examine the images to determine the border between normal and tumor tissue. These images were then used as training data for a machine-learning algorithm, essentially teaching a computer program to distinguish between the pixels in the images that represent normal tissue versus those that represent tumor tissue.
The scientists found that even though 10 out of the 12 test tumors were completely or partly covered by a mucosal layer, the machine-learning analysis was effective in identifying GISTs, correctly color-coding tumor and non-tumor sections at 86% accuracy. “This is a very exciting development,” Dr. Takemura explains, “Being able to accurately, quickly, and non-invasively diagnose different types of submucosal tumors without biopsies, a procedure that requires surgery, is much easier on both the patient and the physicians.”
Dr. Takemura acknowledges that there are still challenges ahead, but feels they are prepared to solve them. The researchers identified several areas that would improve on their results, such as making their training dataset much larger, adding information about how deep the tumor is for the machine-learning algorithm, and including other types of tumors in the analysis. Work is also underway to develop an NIR-HSI system that builds on top of existing endoscopy technology.
“We’ve already built a device that attaches an NIR-HSI camera to the end of an endoscope and hope to perform NIR-HSI analysis directly on a patient soon, instead of just on tissues that had been surgically removed,” Dr. Takemura says, “In the future, this will help us separate GISTs from other types of submucosal tumors that could be even more malignant and dangerous. This study is the first step towards much more groundbreaking research in the future, enabled by this interdisciplinary collaboration.”
For now, a means of accurately and non-invasively detecting GISTs early on could be clinically available widely, soon!
Tokyo University of Science

