Researchers at Baylor College of Medicine found that while most individuals responded to respiratory syncytial virus (RSV) natural reinfection with a typical sustained antibody response associated with protection, a few individuals surprisingly responded atypically, not being able to sustain the antibody response, which declined to levels that made the individuals susceptible to RSV reinfection.
The researchers highlight in their study, published in the journal Vaccine, that their findings point at a subpopulation of people who also may not maintain an antibody response to vaccines and suggest the need to characterize patient-specific responses to respiratory viral infections, such as COVID-19.
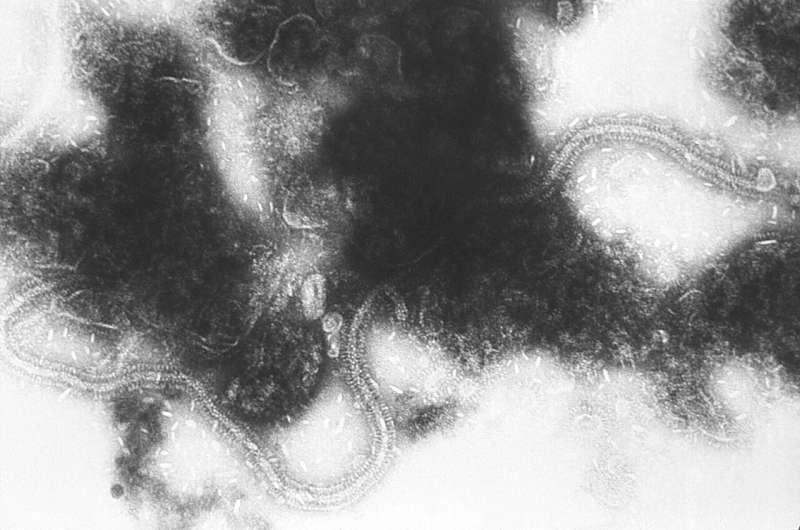
“RSV is the leading cause of childhood acute lower respiratory illness worldwide and a significant cause of morbidity and mortality in older adults,” said corresponding author Dr. Pedro A. Piedra, professor of molecular virology and microbiology, pediatrics and of pharmacology and chemical biology at Baylor. He also is the director of Baylor’s Clinical Laboratory Improvement Amendments (CLIA)-Certified Respiratory Virus Diagnostic Laboratory. Piedra also is a leader in the fight against COVID-19.
In response to RSV infection, the body produces specific antibodies that have been correlated with protection from infection and reduction of severe disease, but reinfection is still frequent.
“To understand RSV reinfection, we studied the levels of the natural RSV-specific antibody response on an adult population during an RVS season in Houston,” said first author Brittani N. Blunck, graduate student in the Piedra lab.
The researchers found that the 19 individuals they studied could be placed in one of three categories according to their antibody profiles: A) those whose RSV antibody profile did not change, an indication that they did not get reinfected during the study period. B) those who showed an increase in RSV antibodies, a typical response showing that they had a reinfection that boosted the antibody response, and C) a surprising, small group that showed good antibody levels at the beginning of the study followed by a quick decline in antibodies to levels that made them susceptible to reinfection.
The ‘original antigenic sin’
“The other important finding was what we call the ‘original antigenic sin,'” Piedra said. “This phenomenon, which has been demonstrated for the influenza virus and others, refers to the immune system responding more to older infections than to recent infections.”
In this original antigenic sin case, the immune system produced a stronger antibody response to RSV strains it had encountered long ago than to other strains of the same virus it encountered more recently.
“That was surprising but not totally unexpected because we see that with other viruses. However, we had not seen that for RSV before,” Piedra said.
“We think that our main findings, the existence of a small portion of a human population that does not sustain an RSV antibody response after reinfection and the original antigenic sin, have important implications for vaccine development and deserve further study,” Blunck said.
“Understanding natural reinfection is essential for vaccine development because it helps us design more effective vaccines,” said co-author Dr. E. Lynn Zechiedrich, Kyle and Josephine Morrow Chair in Molecular Virology and Microbiology at Baylor.
“This study is also relevant to the current COVID-19 epidemic, as in some ways RSV and SASRS-Cov-2 are similar,” said co-author Dr. Brian Gilbert, associate professor of molecular virology and microbiology at Baylor. “We need more detailed studies on the immune responses to SARS-CoV-2, the virus that causes COVID-19.”
The researchers are continuing their studies by investigating the responses of other branches of the immune system, such as the cellular immune response, to RSV reinfection, as well as the mechanism that mediates the atypical antibody response observed in this work.
Baylor College of Medicine

