Researchers within the Biomedicine Discovery Institute at Monash University have made a breakthrough in understanding the role played by high-risk immune genes associated with the development of rheumatoid arthritis (RA).
The findings, published in Science Immunology, were the result of a seven-year collaboration led by Monash University, involving Janssen Research and Development, U.S. and the Karolinska Institute, Sweden.
Certain immune system genes, called Human Leukocyte antigen (HLA)-DR4, cause an increased susceptibility to RA. In this study, using mice genetically modified to express the human HLA-DR4 molecule, the team examined, at the molecular and cellular levels, how T cells recognise these HLA-DR4 molecules. The team also showed that highly similar T cell receptors, likely with similar recognition characteristics, are also present in “RA-susceptible” humans expressing these HLA molecules.
“This suggests that there may be an immune signature of RA development, providing a potential avenue for diagnostic development or a window of opportunity for therapeutic development,” says Dr. Hugh Reid, who co-led the study with Professor Jamie Rossjohn and Professor Nicole La Gruta at Monash University.
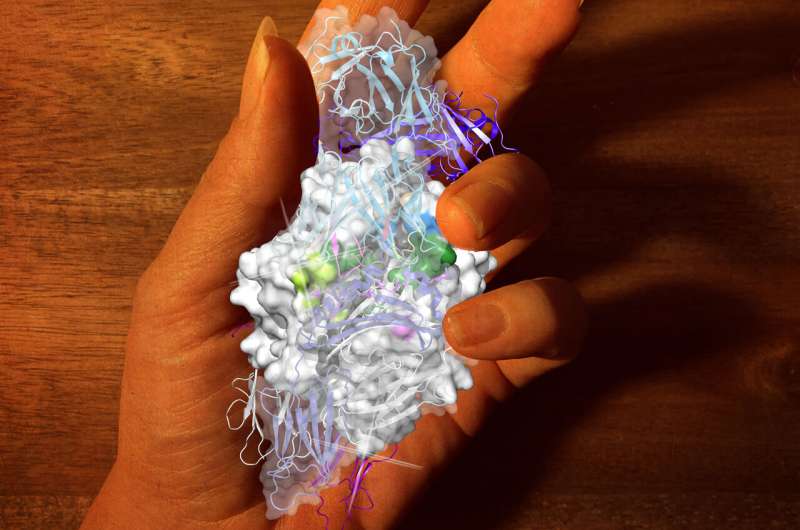
With the assistance of the Australian Synchrotron, the researchers were able to determine the structure of the molecular complexes that form during the interaction between T cell receptors and altered joint proteins bound to HLA-DR4. Armed with this information, they were able to work out what was important in this deleterious T cell response.
“This research is an excellent example of how collaborative efforts between major academic and industrial partners can lead to breakthroughs in basic science that in turn provide avenues for the development of better therapeutics for common diseases,” says Dr. Reid.
Rheumatoid arthritis is an autoimmune disease affecting about one percent of the world’s population. It is characterised by swollen, painful, stiff joints, and consequently, restricted mobility in sufferers. By working out how T cells recognise altered joint proteins in complex with ‘susceptibility’ HLA molecules, Monash scientists have advanced our understanding of how these HLA molecules may predispose individuals to the development of disease. The insight provided may greatly assist in achieving the long-term goal of producing personalised medicines and/or preclinical interventions to treat RA.
Monash University

