Itch torments its sufferers and can be as debilitating as chronic pain.
But it’s a hard symptom to measure—particularly for the 10 million U.S. children with atopic dermatitis, also known as eczema. They can’t always verbalize or quantify their suffering via a survey or scale.
It can also be difficult to objectively measure itch for adults with liver disease, kidney disease and certain cancers who experience its symptoms.
So, it’s hard to track how well treatments and drugs are working.
But now there is a soft, wearable sensor that actually quantifies itch by measuring scratching when placed on the hand developed by Northwestern University scientists. While it was tested in patients with atopic dermatitis, it can be used in any condition that causes itch. The novel sensor can support clinical trials for new treatments, track treatment response and monitor for disease worsening—all in the home setting.
This is the first sensor able to capture all forms of scratching—finger, wrist and elbow motion related. It also is the first validated in a pediatric population where conditions like atopic dermatitis are the most common.
Play00:0000:20MuteSettingsPIPEnter fullscreen
“Itch torments so many patients across so many conditions. It can be as debilitating as chronic pain,” said lead author Dr. Shuai “Steve” Xu, assistant professor of dermatology and of pediatrics at Northwestern University Feinberg School of Medicine. “If we’re able to quantify scratching accurately, then we have the ability to objectively quantify itching. This is really important in patients—like children—who can’t always verbalize or quantify their suffering.”
The paper will be published April 30 in Science Advances.
Xu also is an assistant professor of biomedical engineering at McCormick School of Engineering and Applied Science and medical director of the Querrey Simpson Institute for Bioelectronics, both at Northwestern.
About 10 million U.S. children have atopic dermatitis. The hallmark symptom is itch leading to sleep disturbance, poor neurocognitive development and, on average, a full night of sleep lost per week.
“Atopic dermatitis is so much more than just itchy skin,” Xu said. “It is a devastating disease that causes tremendous suffering worldwide. The quality of life of severe atopic dermatitis (not only for the child but also the parent) is equivalent to many life-threatening diseases.
“Patients with atopic dermatitis are 44% more likely to report suicidal thoughts as a result of the itch compared to controls. Thus, the ability to quantify their symptoms is really important to help new drugs get approved, but also support their day to day lives. In some ways—it’s like measuring glucose for diabetes…measuring itching in an atopic dermatitis patient may be just as important.”
“This is an exciting time for children and adults with atopic dermatitis—or eczema—because of the flurry of activity in developing new therapeutics,” said Dr. Amy Paller, chair of dermatology at Northwestern. “Nothing is more important to measure a medication’s effectiveness for eczema than itch, the symptom that both defines eczema and has the greatest impact on quality of life. This sensor could play a critical role in this regard, especially for children.”
In addition, clinicians and parents have the ability to track how well itch is being controlled in patients at home to monitor for treatment response, as well as early signs of worsening disease, Xu said.
This sensor marries advances in soft, flexible electronics that wrap seamlessly around the hand with machine learning algorithms that specifically identifies scratching without being tricked by similar motion-related movements (e.g. hand waving). The sensor measures both low-frequency motion and high-frequency vibrations from the hand to significantly improve accuracy compared to wrist-watch tools.
The sensor was accepted into the Food and Drug Administration’s Drug Discovery Tool program. This program allows novel devices like this sensor to be qualified to aid in the approval of new drugs.
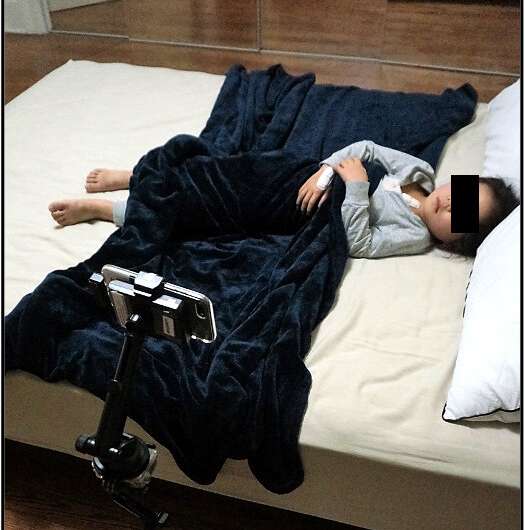
The study was conducted in two parts. The first part involved training the sensor to pick up scratching in healthy adults doing voluntary scratching behaviors. The second part tested the sensors on pediatric patients with atopic dermatitis. Parents set up an infrared camera to serve as the “gold standard”. The algorithm and sensor were then used to count scratches in this pediatric patient population. More than 300 hours of sleep data was manually reviewed and scored for scratching and linked to the sensors.
Northwestern University

