Imagine describing a photograph of an oak tree growing in a meadow. Now imagine describing that same image while a section of your skull has been temporarily removed and a grid of sensors is resting directly on the surface of your brain. These sensors are recording where these electrical signals are rising from your brain. The goal is to create a customized brain map that helps the surgical team remove as much of a brain tumor as possible while minimizing possible damage caused by the physical act of removing the tumor.
You might ask: don’t we already know the functions of the parts of the human brain? Don’t we already have maps that link specific brain functions to particular regions of the brain?
Yes, modern medicine has maps; but human brains are not identical. In addition, the human brain often reorganizes itself in response to damage caused by things like the presence of a growing tumor. This adaptability makes the brain resilient, but it can also make planning tumor removal more difficult. That’s where the sensors come in. When the person speaks and moves while the sensors are running, the surgical team can identify specific areas of the brain that are actually activated while these actions are being performed. This information helps the team build out a map of areas to avoid during the impending surgery.
A University of California San Diego team of engineers, surgeons, neuroscientists, and medical device developers is working together to create better customized maps prior to brain tumor removal surgery. In particular, the team is focused on improving the performance of the flexible mats of sensors that rest directly on the surface of the brain while not puncturing that surface.
These new grids of sensors are also being used to improve epilepsy treatments. For some people with epilepsy, treatment includes surgery where part of the skull is temporarily removed in order to apply gentle electrical stimulation directly to the surface of the brain. The sensor grids developed at UC San Diego are allowing surgical teams to record brain signals while applying the electrical stimulation. Additional work in this area could lead to better epilepsy treatments and perhaps help to uncover the root causes of epilepsy.
Engineers and physicians collaborate
The UC San Diego collaboration between engineers and physicians began more than six years ago, when electrical engineering professor Shadi Dayeh met Eric Halgren, a professor of neurosciences and radiology at UC San Diego Health. The two connected at a mixer organized to introduce engineers at the UC San Diego Jacobs School of Engineering to existing medical challenges and opportunities that might be addressed through engineering.
Fast forward to 2021, and the spark that Dayeh felt as he listened to Halgren’s description of the need for better brain-surface sensors has grown into a dynamic collaboration between the UC San Diego Jacobs School of Engineering and UC San Diego Health. The team has created improved versions of sensor mats that read signals directly from the brain surface during surgery.
Reflecting on their ongoing collaboration, Halgren highlighted how unusual—and welcome—it is to have a partner in engineering who can take a project from conception to clinical application.
https://www.youtube.com/embed/a9uepemE93o?color=whiteCredit: University of California – San Diego
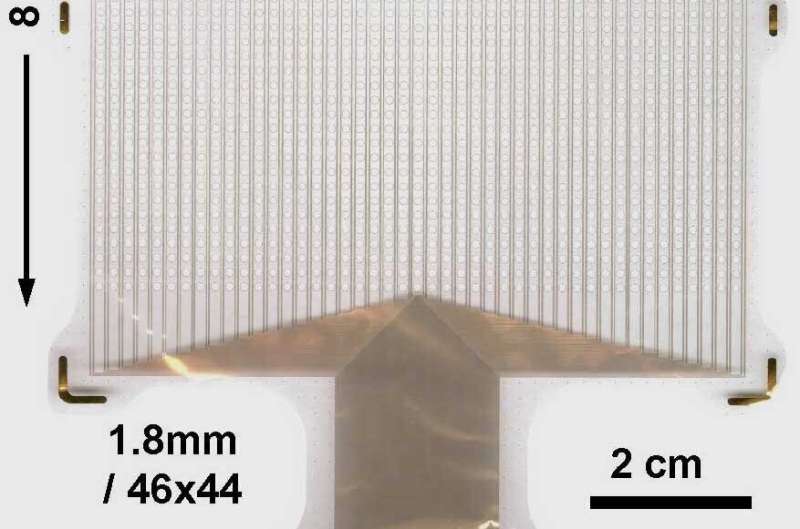
Shadi Dayeh and his team have, in fact, improved these sensor systems in multiple ways, and their work has been used in the operating room. For example, the team has increased the size of the sensor grids and also increased the density of individual sensors within the grids.
While previous generations of these sensors developed elsewhere have been useful in treating patients, “they undersample the brain activity,” said Dayeh, who noted that you can’t just place more existing sensors closer together or shrink existing sensor technologies. “We have turned to advances in materials science to allow us to make small contacts that can be stacked very close to each other. They display low noise, or higher fidelity, in recording these brain signals.”
For both tumor removal and epilepsy treatments, a more tightly packed grid of sensors allows the surgeon to build a higher resolution, custom map of the brain.
In addition to the higher sensor density, the grids that Dayeh and his team create are more supple than other sensor grids. This flexibility allows the sensor grids to more closely follow the undulations of the surface of the human brain, which is important. Closer contact improves signal reading.
“I have been working with professor Dayeh for about six years now, developing advanced neural interface devices. What makes his lab really special is that he is truly doing bench to bedside work,” said Daniel Cleary, a resident physician in the Department of Neurological Surgery at UC San Diego Health in a recent video interview showcasing the Dayeh lab.
“[Dayeh] designs devices using the most advanced engineering materials and electronics work, and then we are able to take those devices and test them in animals and see how well they actually work, revise the devices, and then subsequently take them into the operating room. This is really something special because it represents true translational medicine. There’s a pipeline directly from devices to diagnostic and therapeutic advances,” said Cleary.
Dayeh underscored the value of the partnership.
“Daniel Cleary has been a critical member in the translational efforts across engineering and medicine at UC San Diego,” said Dayeh.
As part of the team’s efforts to translate technological advances into the clinic, Dayeh is engaging the wider community of people who might one day elect to embed—for the long term rather than just during a surgery—devices that interface directly with the brain, the spinal column, or the nerves that extend out across the entire body. Systems that give people who have been paralyzed the ability to not only move limbs but feel what they are grasping are just some of the possibilities.
In an effort to increase public awareness of this work, Dayeh recently joined a conversation with UC San Diego bioethicist Michael Kalichman, who runs a series of public talks called Exploring Ethics. Their video conversation is titled “Neuromodulation: Diagnosis and Therapy for Brain and Spinal Cord Disorders.”
“New technologies, like this one, hold great promise, but success depends on effective dialog with the general public about their worries and needs, as well as strategies to best meet those challenges,” said Kalichman.
The video begins with Dayeh giving a summary of his team’s work and how it fits into the larger research context. Dayeh and Kalichman go on to talk about issues related to the challenges of translating these kinds of technologies into the clinic. People watching the live video stream peppered Dayeh with specific questions about what might be possible by acting directly on the nervous system.
While many of the questions were too specific to be answered by an engineer on a video call, this intense interest from the general public motivates Dayeh’s efforts to ensure everyone is at the table as this work continues. Patient voices and perspectives, for example, were a key part of a 2020 NSF-funded workshop he co-organized. The workshop focused on the current progress and gaps in the clinical translation of devices that interact directly with the brain, the spinal column or the wider nervous system (called “neuromodulation devices”). In particular, the workshop focused on the work being done in universities and startups and aimed to identify the infrastructure needed to fill the identified gaps in university research ecosystems.
Dayeh and his team have formed a startup of their own, with the goal of enabling a wider circle of clinicians to have access to the brain-surface sensor grids they are developing. Along the way, Dayeh intends to keep his work as inclusive as possible. “I think most successful approaches follow the model of involving the end user while designing the system. We do that here.”
University of California – San Diego

