Research led by scientists at Children’s Cancer Institute and published this week in the international journal, Clinical Cancer Research, has found a combination of therapies that appears to be highly effective against high-risk neuroblastoma and other forms of aggressive childhood cancer.
Up to half of all cases of neuroblastoma newly diagnosed in children are ‘high-risk’, meaning the cancer grows aggressively and is difficult to treat. Despite receiving intensive treatment, most children with high-risk disease die within five years of diagnosis, while those who survive are often left with serious long-term health effects.
Professor Michelle Haber AM, a senior author on the paper and co-head of the Molecular Targets and Cancer Therapeutics theme at Children’s Cancer Institute, said children diagnosed with high-risk neuroblastoma have less than a 50-50 chance of survival. “That is a devastating prognosis. We are absolutely determined to find better ways to treat this disease and improve that survival rate.”
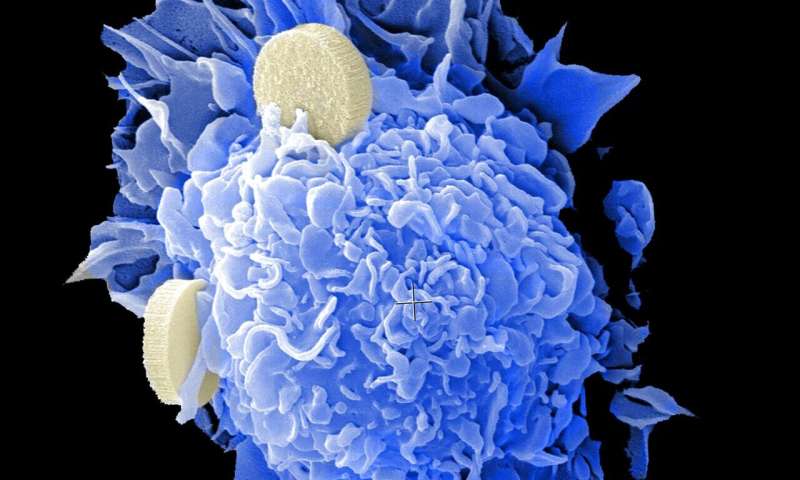
The research focuses on two different types of therapies, both of which have been found to be effective against high-risk neuroblastoma in the laboratory. The first, CBL0137, is a compound called a curaxin, structurally similar to antimalarial drugs. The second is panobinostat, a new type of compound known as a histone deacetylase inhibitor. In the new research, the scientists tested whether the two therapies could work synergistically when used together, each enhancing the anticancer effect of the other.
The researchers found that the two compounds did indeed work well together, effectively inhibiting the growth of cancer cells in culture, as well as in mice bred to develop human high-risk neuroblastoma. As an added bonus, the therapies also jointly acted to heighten the body’s immune response to cancer, which is important since immunotherapy in neuroblastoma is currently challenging.
“In our experiments, we found that the combination of CBL0137 and panobinostat resulted in remarkable growth suppression and an immune response that was tumour-specific,” said Professor Haber. “This is very encouraging, because ideally you want a cancer treatment to specifically target cancer cells and leave healthy cells unharmed, reducing the problem of side effects.”
Dr. Lin Xiao, joint first author and Research Officer in the Experimental Therapeutics Group at the Institute added, “When we used these two compounds together in mice with high-risk neuroblastoma, we saw complete and lasting tumour regression, with minimal ill-effects on the mice. Our results suggest that this combination could work well as a type of immunotherapeutic approach to treating high-risk neuroblastoma.”
Further research at Children’s Cancer Institute has shown that this type of multimodal therapy is also effective against other high-risk childhood cancers, including some forms of brain cancer. Together, it is hoped these results will lead to a new therapy for aggressive childhood cancer.
Children’s Cancer Institute Australia

