Researchers at Baylor College of Medicine have followed the progression of breast cancer in an animal model and discovered a path that transforms a slow-growing type of cancer known as estrogen receptor (ER)+/HER2+ into a fast-growing ER-/HER2+ type that aggressively spreads or metastasizes to other organs.
The study, which appears in the Proceedings of the National Academy of Sciences, has implications for breast cancer therapy as it suggests the need to differentiate cancer subtypes according to the path the cells follow. Different paths might be linked to different cancer behavior, which should be taken into consideration to plan treatment appropriately.
“In general, ER-/HER2+ breast cancer is more aggressive than ER+/HER2+ breast cancer, but the ER- type also is heterogenous in its behavior,” said co-corresponding author Dr. Jianming Xu, Baylor’s Gordon Cain Endowed Professor in Cell Biology in the Department of Molecular and Cellular Biology. “In some patients, the ER-/HER2+ cancer responds to therapy and never returns, but in others, the cancer comes back, grows rapidly, aggressively metastasizes to other organs and does not respond to treatment, which causes death. However, what determines the aggressiveness of individual ER-/HER2+ breast cancer is poorly understood.”
In the current study, Xu and his colleagues investigated the progression of ER+/HER+ and ER-/HER2+ breast cancer cells in a mouse model of the disease. “We wanted to know whether the diversity in cancer behavior was related to where the cells came from,” said Xu, a member of Baylor’s Dan L Duncan Comprehensive Cancer Center.
Following the path of cancer
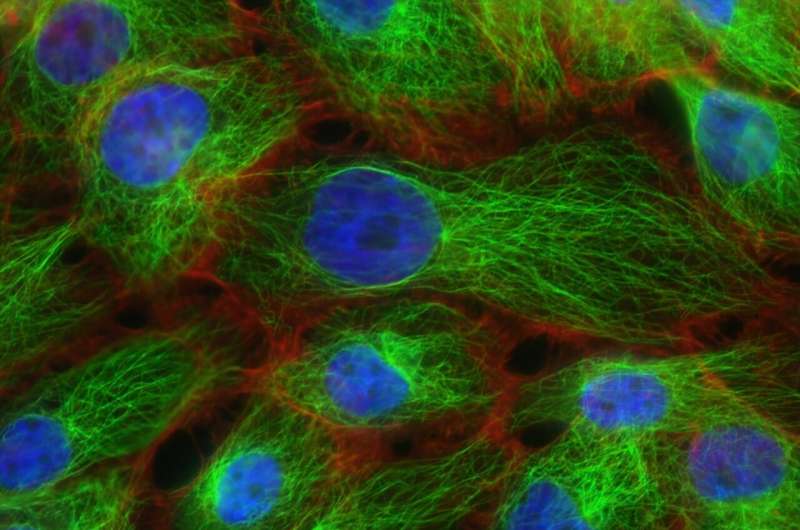
The researchers applied a novel approach setting up a mouse model in which they could follow the ER+/HER2+ and the ER-/HER2+ cancer cells from the beginning of tumor growth through its progression as it became metastatic in living animals. They traced all tumor cells arising from ER+ cells with a red fluorescent protein they could detect during the entire progression. The team also compared ER expression, cell proliferation and metastatic capability among the different subtypes of breast cancer cells that emerged during the process.
The animal model began with equal parts of ER+/Her2+ and ER-/HER2+ breast cancer cells. As the cancer grew, the ER-/HER2 cells, which proliferated rapidly but metastasized little, only gave rise to more ER-/HER2+ cells with similar behavior. On the other hand, although the ER+/HER2+ cells produced mostly slow-growing ER+/HER2+ cells, some ER+/HER2+ cancer cells generated cells that had lost their ER. This new population of ER-/HER2+ cancer cells grew rapidly and spread to other tissues aggressively.
“Our study proposes that the fast-growing ER-/HER2+ cancer cells can be divided into two subtypes, one that has an ER+ origin, grows quickly and metastasizes aggressively, and another that has an ER- origin and also grows fast but has a less aggressive metastatic behavior,” Xu said. “Currently, all ER-/HER2+ breast cancers are treated in the same way and produce diverse responses. Our findings suggest that different treatments might be in order. If the observations in our animal model can be validated in humans, we would anticipate that ER-/HER2+ cancer with an ER+ origin would be very aggressive and should be treated accordingly, while the ER-/HER2+ cancer that originated from ER- cells would tend to be less metastatic and therefore would require a different treatment.”
Looking into what mediates different behavior in ER-/HER2+ breast cancer
The team also investigated why the ER-/HER2+ cancer cells derived from ER+ cells had lost the ER marker and what might have triggered their aggressive metastatic behavior. “We compared ER-/HER2+ cancer cells of ER+ origin, the most aggressive type, with normal ER+ mammary gland cells from where these cancer cells had originated, at the DNA level,” Xu said. “We found that the most aggressive cancer type, but not the other, had changes in the DNA that led to shutting down ER expression, which provided an explanation for why the cells had lost their ER.”
Xu and his colleagues also looked to explain why the origin of ER-/HER2+ cancer cells would make a difference in the cells’ metastatic behavior. They discovered that the activation of a key enzyme called MAP kinase was different between the most aggressive and the less aggressive ER-/HER2+ cells, and they propose that this difference provides an answer to the nature of their behavior.
“These findings encourage us to investigate whether the discoveries we have made in an animal model also occur in patients with breast cancer,” said co-corresponding Dr. Bert O’Malley, professor of molecular and cellular biology and chancellor at Baylor. He also is a member of the Dan L Duncan Comprehensive Cancer Center. “Our study supports the concept that cancer progression involves dynamic changes in the cancer cell population. We need to understand these changes so we can design therapies that play along with them to improve the outcomes of this devastating disease.”
Baylor College of Medicine

