In a consensus guideline issued by the Global Interventional Inflammatory Bowel Disease Group and published in the June 1 issue of The Lancet Gastroenterology & Hepatology, recommendations are presented for endoscopic evaluation of surgically altered bowel in inflammatory bowel disease.
Noting that most patients with Crohn disease and some with ulcerative colitis will require surgical treatment, despite advances in diagnosis, therapy, and endoscopic interventions, Bo Shen, M.D., from the Columbia University Irving Medical Center in New York City, and colleagues developed recommendations for evaluation of surgically altered bowel.
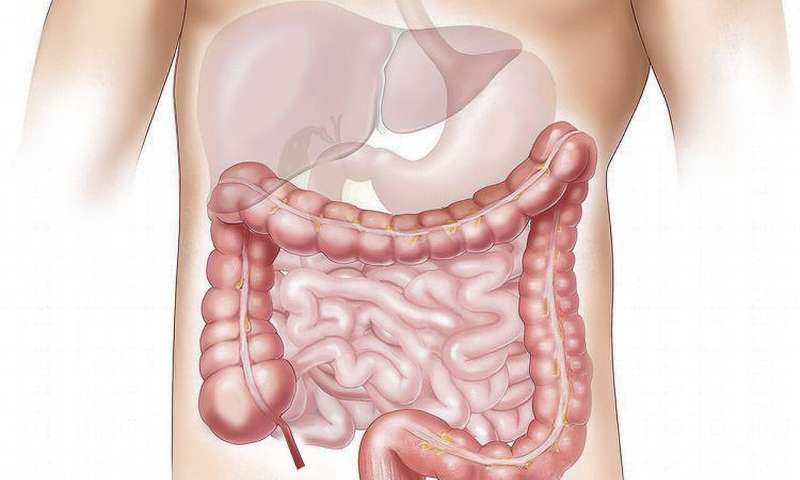
The authors note that bowel resection with anastomosis, strictureplasty, fecal diversion, and ileal pouch are among the most commonly performed surgical procedures. Endoscopy plays a key role in assessment of disease activity, disease recurrence, treatment response, dysplasia surveillance, and delivery of endoscopic therapy among patients with inflammatory bowel disease. Owing to loss of bowel reserve, changes in bowel anatomy, intrinsic or extrinsic partial obstruction, and patients’ poor nutritional status and use of immunosuppressive medications, endoscopic evaluation of surgically altered bowel can be challenging. Patients with a surgically altered bowel usually need a multidisciplinary team approach to address the complexities in diagnosis and management of inflammatory bowel disease.
“In this consensus guideline we have outlined anatomies frequently seen at endoscopy in the surgically altered bowel in healthy and diseased states, and have provided principles and techniques of endoscopy in these patients,” the authors write.
Several authors disclosed financial ties to the biopharmaceutical industry.
HealthDay