More than a third of coal miners and former coal miners suffering from black lung disease struggle with depression, and more than one in 10 has recently considered suicide, a new study finds.
The study is believed to be the first to examine mental health issues in a large population of coal miners in the United States. Based on the troubling results, the researchers are calling for more mental health resources and treatment for current and former miners. They also are urging further study of potential contributors to the problem, including social determinants of health, substance use and workplace safety.
“Although coal mining is on the decline, the rates of black lung in Southwest Virginia continue to increase. Coal miners in Central Appalachia face disparities in health related to a range of complex social, economic, occupational and behavioral factors,” said researcher Dr. Drew Harris, a pulmonary medicine expert at UVA Health. “This study highlights the unrecognized crisis of mental illness in miners that warrants urgent attention, resources and expanded care.”
Miners’ Mental Health
Harris serves as the medical director of the Black Lung Clinic at Southwest Virginia’s Stone Mountain Health Services, the only federally funded black lung clinic in Virginia. Black lung is a progressive lung illness caused by inhaling toxic coal and rock dust within coal mines. The dust literally blackens the insides of the lungs and leaves patients struggling to breathe. This devastating disease has few treatment options and is increasingly being diagnosed in Central Appalachian coal miners: Out of more than 1,400 coal miners X-rayed in the last year at Stone Mountain, more than 15% had progressive massive fibrosis, the most severe form of black lung.
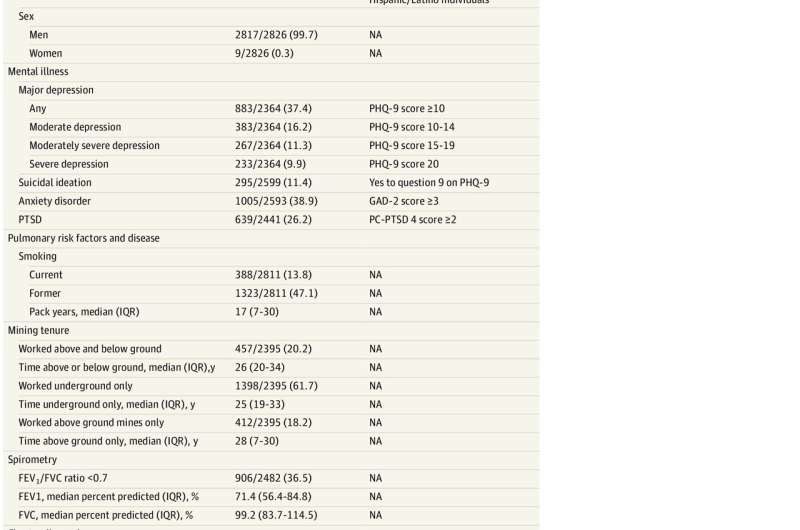
To gauge the mental wellbeing of black-lung patients, Harris and his colleagues reviewed data collected at the clinic since 2018 assessing patients for anxiety, depression and post-traumatic stress disorder.
More than 2,800 miners voluntarily completed a mental-health survey. The average age was 66; 99.6% were white; and 99.7% were male.
Of the participants:
- 883 patients, or 37.4%, reported symptoms consistent with major depressive disorder.
- 1,005 patients, or 38.9% had clinically significant anxiety.
- 639 patients, or 26.2%, had symptoms of PTSD.
- 295 patients, or 11.4%, had considered suicide in the last year. (For comparison, this figure is only 2.9% among Virginia men overall.)
“These rates of mental illness far exceeded those documented in coal mining populations internationally,” the researchers write in a new scientific paper outlining their findings.
Rates skewed highest among sicker patients who required supplemental oxygen to help them breathe. Among that group, 47.7% reported anxiety, 48.5% reported depression and 15.9% reported considering suicide.
The researchers note that depression and other mental health issues not only affect patients’ quality of life, but can reduce the likelihood they will stick with their medications.
“The rates of mental illness identified in this large population of U.S. coal miners is shocking,” Harris said. “Improved screening and treatment of mental illness in this population is an urgent, unmet need that warrants urgent action.”
The researchers have published their findings in JAMA Network Open.
Josh Barney, University of Virginia

