A presentation at this year’s European Congress on Clinical Microbiology & Infectious Diseases (ECCMID), held online this year, will discuss the growing evidence that the beta SARS-CoV-2 variant first identified in South Africa is leading to more severe disease in people living with HIV, and that failure to clear SARS-CoV-2 infection in a patient with advanced HIV creates conditions that can lead to evolution of dangerous mutations in SARS-CoV-2.
Control of HIV with antiretroviral therapy could be the key to preventing such evolution of SARS-CoV-2 in patients with advanced HIV, since clearance of the virus is compromised if HIV is allowed to replicate for a long time and results in major damage to the immune system.
“Evolved mutations lead to escape from neutralisation, which means antibodies made as a result of previous natural infection or vaccination would work less well to protect you from a new infection,” explains session presenter Dr. Alex Sigal, Africa Health Research Institute, KwaZulu-Natal, South Africa, and Max Planck Institute for Infection Biology, Berlin, Germany. “SARS-CoV-2 may mutate extensively within one person if infection persists.”
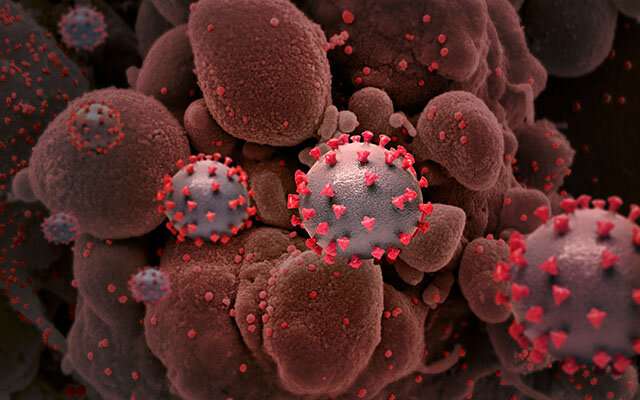
In his talk, Dr. Sigal will present a case study of a patient with advanced HIV who, despite having only mild COVID-19 illness, tested SARS-CoV-2 positive for 216 days. Genomic sequencing revealed shifts in the patient’s SARS-CoV-2 viral population over time, involving multiple mutations at key sites including the spike protein domain which SARS-CoV-2 uses to enter human cells. The evolved virus was tested and shown to have variant-like properties in terms of its ability to escape antibodies.
“Such findings underline the need to make sure everyone living with HIV has appropriate treatment. If not, it is possible that potentially more potent variants than the ones circulating now could emerge from people whose immune systems are severely damaged,” he explains.
European Society of Clinical Microbiology and Infectious Diseases

