A new report from the long-term ASPREE study, involving Monash University, has revealed high blood pressure variability (BPV) in older adults, particularly in men, is associated with an increased risk of dementia and cognitive decline.
Published in the Journal of the American Heart Association, the findings may identify people at increased risk of major cognitive impairment, allowing for triage into heightened surveillance, and point the way to new areas for research.
The new paper is one of many important health findings yielded from the ASPREE (ASPirin in Reducing Events in the Elderly) dataset. The primary prevention aspirin trial released main results to global acclaim in 2018. Further analysis of the extensive, high quality data from 19,114 Australian and Americans, continues to drive new findings in healthy older adults, mostly over the age of 70.
This study was co-led by Associate Professor Joanne Ryan from the Monash School of Public Health and Preventive Medicine and Professor Mike Ernst from the University of Iowa.
“By around 2050 we believe that people aged 60 years and older will outnumber adolescents and youths. As an age‐related disease, and one with a notable lack of treatments, dementia will indefinitely remain a major public health priority,” Associate Professor Ryan said.
“Any opportunity to identify early those at risk, and engage people in preventive therapies, is important.”
Hypertension—systemic high blood pressure—in mid-life has previously been shown to be a strong predictor of dementia in later life. More recently, data has shown that more granular short and long-term fluctuations in blood pressure (BPV) are also an indicator of cognitive decline.
However, most studies investigating BPV involved younger people, older people already diagnosed with cognitive impairment, or used a single cognitive assessment tool to gauge cognitive acuity.
“The ASPREE dataset was uniquely suited to provide a robust answer to this question; a large cohort of participants underwent standardised blood pressure and cognition assessments, and they received long-term follow up,” says Associate Professor Ryan.
“Importantly, rather than just a single cognitive assessment tool, participants underwent a series of cognitive tests. This enabled us to capture detail on many facets of cognition and memory, including global cognition, delayed episodic memory, verbal fluency, and processing speed and attention.
“They also underwent a validated depression scale prior to each annual cognitive test, which is important because depression may have an impact on cognitive function.”
Blood pressure was recorded for all participants during their annual visits, and was done so in accordance with guidelines from the American Heart Foundation.
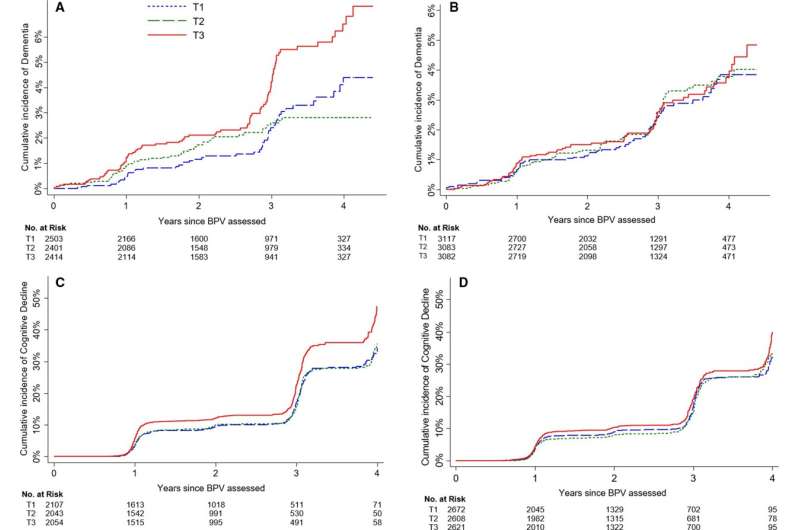
Data from 16,758 participants were included in this study. The researchers grouped participants at baseline (study entry) into three groups, based on BPV: low, medium and high. BPV was generally higher among women than men, but cognitive scores were similar across participants with low, medium and high BPV.
Over time, differences emerged. Those in the highest BPV group were shown to be at significantly increased risk of incident dementia and cognitive decline compared with those in the lowest BPV group. Being male also increased the risk significantly.
The findings support the earlier results that had suggested BPV may be a useful indicator of cognitive decline, expanding our understanding to include older, relatively healthy adults who had reached late life without significant cognitive impairment—a group that is not typically considered at high risk for dementia in their remaining lifespan.
The results also provide the first evidence of possible sex‐specific effects of BPV on cognition.
The biological mechanisms underpinning the relationship between BPV and cognitive decline remain unclear, and the researchers say this should be a focus of further investigation.
Accumulating evidence suggests BPV is associated with structural brain changes, including increased lesions in the brain called white matter hyperintensities, increased small bleeds in the cerebrum, and enlarged fluid-filled spaces in the brain matter. Whether these changes are caused by BPV or vice versa is unknown.
Degeneration of neurons and synapses associated with Alzheimer’s disease may influence the body’s regulation of blood pressure, which may contribute to increased BPV. This may cause a loop, whereby microvascular damage from blood pressure instability might alter the permeability of the blood brain barrier, enabling accelerated damage to brain neurons. While all ASPREE participants were without symptoms of cognitive impairment at study entry, some may have had pre-symptomatic established disease that contributed via this pathway.
Men have a higher lifetime exposure than women to other known risk factors of cognitive decline, such as uncontrolled high blood pressure and smoking. But even when the researchers accounted for those, the increased risk for men remained.
Associate Professor Ryan said: “While we don’t know for sure, it is tempting to speculate about the existence of different pathways towards cognitive decline in men and women. Or sex hormones such as oestrogen across a woman’s lifetime may have a protective effect for women.
“More study is warranted into this area to help determine the underlying reasons for these sex-specific differences, and into research to find out whether reducing BPV can preserve late-life cognitive function.”
The paper, published in Journal of the American Heart Association, is titled “Long-Term Blood Pressure Variability and Risk of Cognitive Decline and Dementia Among Older Adults.”
Monash University

