By some estimates, 2 billion people are now infected worldwide, and in 2019, around 1.4 million people died from it.
It’s a pandemic infection, spread through the air—but it’s not COVID. It’s tuberculosis (or TB). Yet we’re not in lockdown for it. And we’re not queuing up for a vaccine.
Some people call TB “the forgotten pandemic”. But our knowledge of one pandemic is helping us manage the other.
They’re similar in some ways …
TB is caused by the bacterium Mycobacterium tuberculosis. And COVID is caused by SARS-CoV-2, a virus. They’re quite different microorganisms. But it’s easy for them to overlap in people’s minds.
Both TB and COVID are infectious diseases that generally affect the lungs. Both are passed between people mainly by aerosols, when infected people cough, sing or otherwise release them into the surrounding air.
So some of the things we’re used to doing for COVID-19—like wearing masks and good ventilation—also work for preventing the spread of TB.
However, there are some important differences between them, which mean our public health responses can look quite different.
… but not in others
We are all so familiar with COVID. So when I’m talking with people about TB, I’ve started highlighting three key differences between the infections.
1. TB is less infectious
TB is much less infectious. While COVID (especially strains like the Delta variant) may be transmitted after brief or “fleeting” contact, this is rare for TB.
As a rule of thumb, TB programs around the world often suggest you need to be in close contact with an infectious person for more than eight hours before that risk builds up to the point where you need to be tested for it.
This means people are more likely to spread the infection within their household or immediate family rather than at the shops.
2. TB symptoms take longer to show up
With TB, the “window” between being exposed and becoming unwell, known as the incubation period, is much longer.
Infections can stay dormant (or “latent”) in the body for many months or years before people become unwell. But almost everyone who becomes unwell with COVID has been infected within the past two weeks.
https://platform.twitter.com/embed/Tweet.html?dnt=false&embedId=twitter-widget-0&features=eyJ0ZndfZXhwZXJpbWVudHNfY29va2llX2V4cGlyYXRpb24iOnsiYnVja2V0IjoxMjA5NjAwLCJ2ZXJzaW9uIjpudWxsfSwidGZ3X2hvcml6b25fdHdlZXRfZW1iZWRfOTU1NSI6eyJidWNrZXQiOiJodGUiLCJ2ZXJzaW9uIjpudWxsfSwidGZ3X3NwYWNlX2NhcmQiOnsiYnVja2V0Ijoib2ZmIiwidmVyc2lvbiI6bnVsbH19&frame=false&hideCard=false&hideThread=false&id=1397504069917319170&lang=en&origin=https%3A%2F%2Fmedicalxpress.com%2Fnews%2F2021-08-tuberculosis-forgotten-pandemic-year-old-vaccine.html&sessionId=1a6a66def3920f4ecfbf66afa0f431c08632c648&theme=light&widgetsVersion=1890d59c%3A1627936082797&width=550px
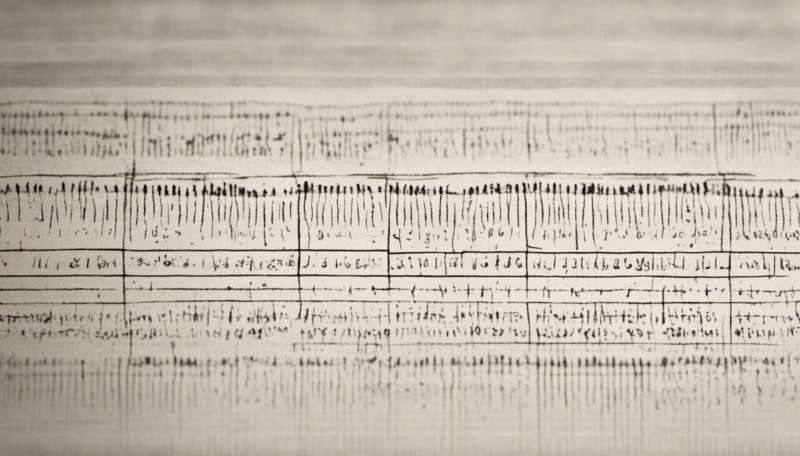
#Tuberculosis is the most common cause of infection-related death worldwide. World Health Organization declared TB to be a global public health emergency. The image below depicts typical radiographic findings on a patient with tuberculosis.#Pediatric anesthesia and critical care pic.twitter.com/0798mKz1rw— Pediatric Anesthesia And Critical Care (@and_pediatric) May 26, 2021
We don’t ask contacts of TB to isolate at home as we can’t predict when they might become unwell. It certainly wouldn’t be ethical or realistic to isolate people for months or years, just in case. Fortunately, people who have dormant TB cannot pass infection on to others in the meantime.

3. We have TB treatments to help curb the spread
As we’re uncertain about how long it takes between someone becoming infected and becoming unwell with TB, you’d think that would be a big problem.
But we have effective treatments to give people with dormant TB. These help prevent them developing active disease.
These treatments, particularly antibiotics such as isoniazid or rifampicin, can greatly reduce the risk of contacts becoming sick.
For COVID, we don’t yet have any treatments for people who are infected but who are not showing symptoms (known as post-exposure treatments) to minimize the chance of them spreading the virus.
Some have been tried, but so far none have convincingly been shown to be effective.
How about vaccines?
Perhaps the biggest difference in our response to these pandemics is we have a variety of effective vaccines against COVID.
For TB, we are relying on a 100-year-old vaccine, known as BCG (short for Bacille Calmette-Guerin), which is still one of the most widely used vaccines globally.
While it protects young children from the most severe forms of TB, the vaccine seems to give much less protection for adults.
The BCG vaccine, unlike COVID vaccines, is a live vaccine, meaning it contains live (but weakened) bacteria. So it can’t be given safely to people with immune suppressing conditions, like HIV, because they could get infected from it. This means its use is limited in some people who most need protection.
TB vaccine may protect against COVID
Perhaps the BCG vaccine and COVID will come full circle. The BRACE trial, launched from Melbourne’s Murdoch Children’s Research Institute, is studying whether the BCG vaccine might protect against COVID infection.
This investigation has been prompted by a long history of research showing the vaccine also improves our immune responses to other conditions such as viral infections.
We don’t know yet whether this will work, as the study is ongoing. Almost 7,000 health-care workers around the world at risk of COVID exposure have been recruited to the trial.
Whether or not BCG turns out to prevent COVID, there’s no question we need new and more effective vaccines for TB.
While we have an increasing number of potential vaccine candidates, right now there is still no alternative to our 100-year-old BCG.
The massive amount of activity globally in developing COVID vaccines has also stimulated calls for greater efforts and funding to develop new TB vaccines.
We hope these will lead to more effective and safer options, and be powerful tools for eliminating TB. Let’s hope we’re not left waiting another 100 years.
Justin Denholm, The Conversation

