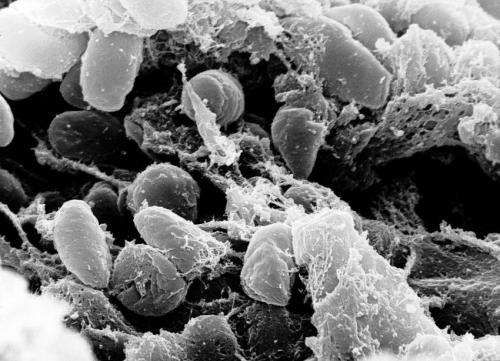
Although the world is focused on the COVID-19 pandemic, there are many other dangerous pathogens still out there, like Yersinia pestis, which causes plague—the deadly disease that killed tens of millions of people during the infamous Black Death in the 14th century. Although plague has been largely eradicated in the developed world, it still affects hundreds of people globally each year.
When a human is infected with bubonic plague from a flea bite and it goes untreated, the infection can progress and spread to the lungs, resulting in pneumonic plague. The most feared clinical form of plague, pneumonic plague is typically lethal if not quickly treated, and infected patients can transmit the disease to others via respiratory droplets. A team of scientists from Northern Arizona University’s Pathogen and Microbiome Institute, led by professor Dave Wagner, recently published their findings from a remarkable study involving antimicrobial resistant (AMR) plague.
Although pneumonic plague outbreaks are now extremely rare, scientists consider plague to be a reemerging and neglected disease, particularly in the East African island country of Madagascar, which reports the majority of annual global cases. With no vaccine against it, preventing mortality from plague requires rapid diagnosis followed by treatment with antibiotics. An AMR strain of Y. pestis—resistant to the antibiotic streptomycin, usually the first-line treatment for plague in Madagascar—was isolated from a pneumonic plague outbreak that occurred there in 2013, involving 22 cases, including three fatalities.
Wagner’s team, including PMI senior research scientists Dawn Birdsell and Nawarat Somprasong, PMI assistant director Amy Vogler, professor Herbert Schweizer, associate professor Jason Sahl and senior research coordinator Carina Hall, conducted a study of this outbreak, together with long-term research partners at the Institut Pasteur de Madagascar and scientists at the Institute Pasteur Paris and the Madagascar Ministry of Public Health. The results of the study, “Transmission of antimicrobial resistant Yersinia pestis during a pneumonic plague outbreak,” were recently published in the journal Clinical Infectious Diseases.
“By characterizing the outbreak using epidemiology, clinical diagnostics and DNA-fingerprinting approaches,” Wagner said, “we determined—for the first time—that AMR strains of Y. pestis can be transmitted person-to-person. The AMR strain from this outbreak is resistant to streptomycin due to a spontaneous point mutation, but is still susceptible to many other antibiotics, including co-trimoxazole. Luckily, the 19 cases that were treated all received co-trimoxazole in addition to streptomycin, and all of them survived.
“The point mutation, which also is the source of streptomycin resistance in other bacterial species, has occurred independently in Y. pestis at least three times and appears to have no negative effect on the AMR strain, suggesting that it could potentially persist in nature via the natural rodent-flea transmission cycle. However, AMR Y. pestis strains are exceedingly rare and the mutation has not been observed again in Madagascar since this outbreak.”
Northern Arizona University

