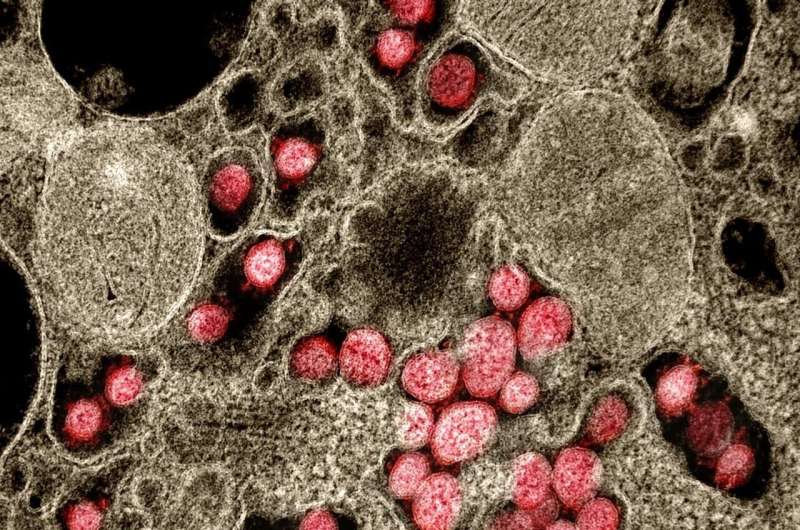
Age is the primary risk factor for many infectious diseases including COVID-19. A team of researchers led by CiRA Prof. Yoko Hamazaki shows in a new study that changes in the quantity and quality of killer T cells with age is consistent with older populations showing more severe COVID-19 symptoms.
The rapid spread of the new coronavirus, SARS-CoV-2, and the COVID-19 pandemic associated with its infection has led to a monumental effort by scientists around the world to understand and treat the disease. It was immediately apparent that older populations were susceptible to the respiratory problems caused by the virus, with people above 75 years old being several hundreds of times more likely to die than someone in their 20s.
Hamazaki explains the vulnerability to infectious disease in older populations is partly due to the aging of our immune systems.
“Something that happens in all our bodies with age is thymic involution. This leads to a decrease in new naive killer T cell production, subsequently a change in their quantity and quality and how our immune system fights off infection,” she said.
Killer T cells are essential immune cells for eliminating cells infected by viruses. Scientists have categorized them into naïve, memory and effector types. The effector type is most effective at attacking a pathogen, whereas the naïve type expands the number of effector T cells and create immunological memory. Naïve killer T cells are also needed by the body to respond to new pathogens, such as SARS-CoV-2.
The study looked at two different cohorts of Japanese populations by sampling blood from 30 young people (average 22 years old) and 26 old people (average 72 years old) who had never been infected with SARS-CoV-2 and tested how T cells from these samples could react to the virus. The number of killer T cells that reacted to SARS-CoV-2 were similar between the two groups. However, consistent with thymic involution, the researchers found the number of naïve killer T cells that reacted were far fewer in the blood samples from the older cohort.
Interestingly, memory and effector killer T cells that react to SARS-CoV-2 already exist in our bodies because of exposure to common-cold corona viruses. “However, those in the elderly population showed a more senescent phenotype with high effector function but less proliferation capacity,” said Hamazaki, suggesting the killer T cell populations are able to fight SARS-CoV-2 in a short period, but the effects cannot be well maintained.
Furthermore, she and her research team found that even the young cohort could be divided into two populations. Almost half of young subjects showed more killer T cells with the same senescent phenotype as the older cohort. These subjects were all positive for a previous infection by cytomegalovirus, a common virus that normally causes no symptoms in infected people.
The findings suggest that not only age, but also past infections influence how the body responds to the new coronavirus.
Overall, Hamazaki believes that recognizing the size and constituency of a killer T cell population before SARS-CoV-2 infection could act as predictor of COVID-19 risk.
“Normally, the disease first causes mild symptoms in elderly patients before advancing to severe symptoms. This could reflect the presence of effector killer T cells that initially fight the infection, but naïve T killer cells not expanding into new effector cells,” she said.
Hamazaki also said that in addition to increasing antibodies against SARS-CoV-2, “the expansion of killer T cells after vaccination could be a key to enhancing immunity in the elderly.”
Kyoto University

