Rheumatoid arthritis (RA) is an autoimmune, inflammatory disease. Though the precise mechanism of the disease is only partially understood, people with RA produce antibodies that target their own tissues, contributing to painful inflammation in the joints that can cause bone loss.
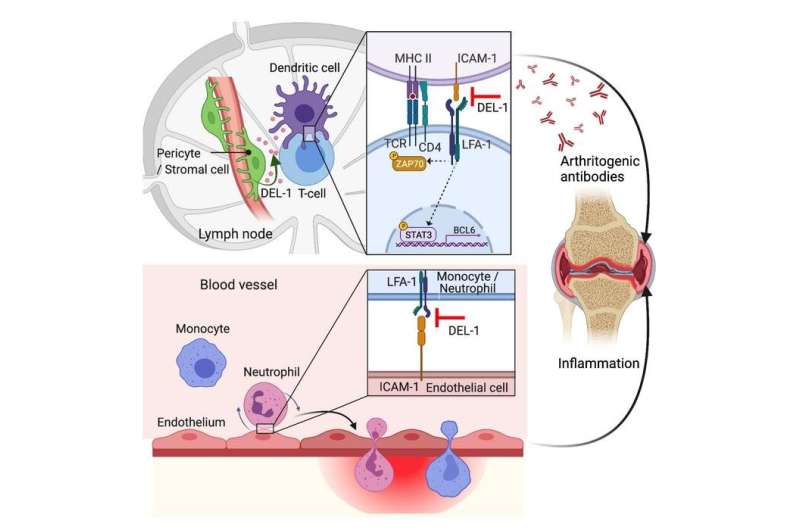
In a new study published in the Journal of Clinical Investigation, researchers from the University of Pennsylvania School of Dental Medicine found that the molecule DEL-1—already known to protect against periodontitis and other inflammatory diseases in animal models—similarly offers protection from the joint-damaging inflammation of RA. Using two distinct models of RA, the team, led by George Hajishengallis of Penn and Triantafyllos Chavakis of Germany’s Technical University of Dresden, showed that DEL-1 acted in two ways: in the joints themselves, preventing immune cells from fostering inflammation, and in the lymph nodes, interfering with the production of joint-damaging antibodies.
“We find that DEL-1 has a dual action,” says Hajishengallis, “both preventing the induction of autoantibodies, which is a totally new mechanism but also restraining the recruitment of inflammatory cells in the joints. I think that DEL-1 could be a very, very valuable therapeutic for rheumatoid arthritis, though we’ll need support for clinical trials in humans to test this.”
Hajishengallis’ and Chavakis’ labs have extensively studied DEL-1 for years in other inflammatory conditions, including periodontitis, a severe form of gum disease, and multiple sclerosis, a disease of the central nervous system. They’ve shown that DEL-1 can restrain the initiation of inflammation and also resolve ongoing inflammation, depending on the context and location in which it is expressed. “This is another example of the functional versatility of DEL-1 based on its compartmentalized expression,” says Chavakis.
Knowing that inflammation is the critical contributor to pathology in RA as well, they sought to test whether and how DEL-1 was at work in this new disease context.
“Despite differences in their etiology, rheumatoid arthritis is similar to periodontitis in that they both are bone-loss disorders,” says Hajishengallis.
To start, the researchers looked at mice that had been bred to lack DEL-1 and found that, compared to genetically normal mice, they were far more susceptible to inflammatory arthritis, pointing to a protective role for DEL-1.
To see if enhancing DEL-1 levels could shield animals from severe disease, the team next examined mice bred to overexpress DEL-1 only in their endothelial cells, which they had previously found to be involved in preventing recruitment of inflammatory immune cells. These animals, they found, had less severe disease in two different models of inflammatory arthritis and had lower abundance of recruited macrophages and neutrophils in their joints as well.
“That meant DEL-1 confers protection against arthritis at least in part by restraining recruitment of inflammatory cells,” Hajishengallis says. “That was expected based on our previous work; it wasn’t something new.”
What did come as a surprise, however, were the differences they saw between the two mechanisms of inducing disease when they studied mice bred to overexpress DEL-1 in mesenchymal stromal cells including fibroblasts, cells in connective tissue that are involved in the disease processes of RA. In one disease model, the researchers directly administered antibodies against collagen in the mice, leading to inflammatory arthritis. But in the other model, collagen is administered, and the mice make the antibodies that target collagen themselves.
In their experiments with DEL-1 overexpressed in fibroblasts, they saw that mice immunized with collagen were protected from severe joint inflammation. But mice that received antibodies directly were not protected. The result was so unexpected that Hajishengallis asked postdoc Hui Wang, the study’s first author, to repeat the experiment. But he came up with the same result: no difference between the DEL-1 overexpressing mice and their genetically normal littermates.
“That got us thinking that DEL-1 might be doing something related to the production of antibodies, not just the restraining of immune cells,” Hajishengallis says.
To test whether this new hypothesis was correct, they went back to blood samples they had taken from the earlier experiments and found that, when immunized with collagen, genetically normal mice produced greater numbers of antibodies in their blood than mice with DEL-1 overexpressed in mesenchymal stromal cells.
But how was DEL-1 influencing antibody production? To find out, they looked in the lymph nodes, where dendritic cells present bits of protein they’ve taken up to T cells, which themselves become specialized to help B cell produce antibodies. Through a series of experiments in cells in culture, the researchers found that DEL-1 did not act on T cells or B cells directly; rather, it blocks the interaction between dendritic and T cells.
Dendritic cells activate a receptor on T cells called a LFA1 integrin, which contributes to the evolution of a so-called “naïve” T cell into a specialized helper T cell named “follicular,” which plays a role in antibody formation.
Turning back to their animal model, the research team wanted evidence that DEL-1 was indeed acting in the lymph nodes to block this interaction. “And indeed, we found DEL-1 in the right region, produced by perivascular stromal cells,” says Hajishengallis.
Taken together with other previous work on DEL-1 and inflammatory conditions, the new findings lend support to the idea that DEL-1 itself could be a therapeutic in RA and perhaps other contexts, or that low DEL-1 levels could serve as a diagnostic for RA, a disease that is frequently a challenge to diagnose.
“The more genetic tools we have to investigate the role of DEL-1, the more we learn about how it is acting in these inflammatory conditions,” Hajishengallis says. “We’re hoping to capitalize on these discoveries in the future.”
Katherine Unger Baillie, University of Pennsylvania

