Scientists have discovered a new link that could bring the scientific and medical community closer to understanding why glioblastoma, the most common malignant brain tumor, is deadlier in males than females.
A new study by Florida International University’s Robert Stempel College of Public Health & Social Work, Cleveland Clinic Lerner Research Institute, and the National Cancer Institute, part of the National Institutes of Health, reveals for the first time a connection between translocator protein 18 kDa (TSPO), a widely used biomarker of neuroinflammation, and survival outcomes in glioblastoma patients. Findings suggest that a variation in the protein’s structure correlates with worse survival outcomes in males than females. The study was published in the September special issue “Infiltrative Gliomas: Emerging Insights into Pathophysiology, Diagnosis, and Management” of the Cancers journal.
“This is a fascinating observation because glioblastoma has sex-specific differences,” said Diana Azzam, assistant professor at Stempel College, who was corresponding author of the study. “It’s more frequent in males than females, and the survival outcome of males is worse than females. In the future, this can potentially help patients receive personalized treatments for the disease.”
Azzam worked closely with the study’s lead authors Katie M. Troike, Ph.D. candidate in the Molecular Medicine Ph.D. program at Cleveland Clinic, and Arlet M. Acanda de la Rocha, a postdoctoral associate at Stempel College.
“I’ve studied TSPO for more than 20 years and knew that it was highly expressed in glioblastomas. This outstanding research team is beginning to uncover its role in one of the deadliest cancers,” said Tomás Guilarte, scientist, professor and dean of Stempel College, who was a senior author of the study. “We hope this research will lead to finding better treatments and, one day, a cure.”
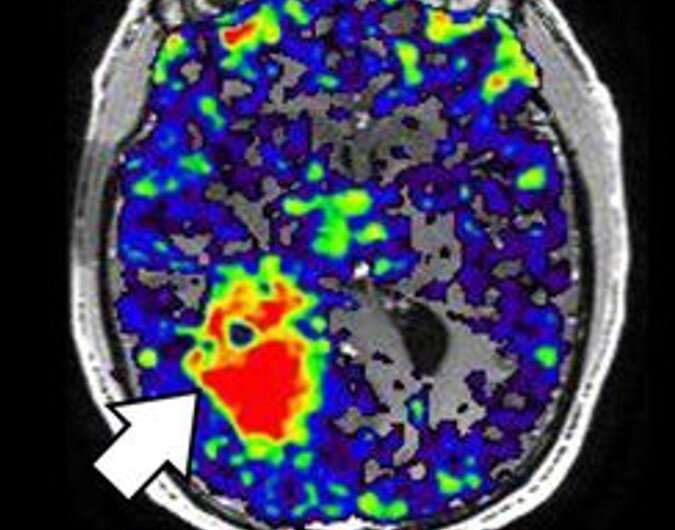
Glioblastoma is found in adults and is 1.6 times more likely to affect males than females. Each year, approximately 12,000 people in the U.S. are diagnosed with glioblastoma. Patients diagnosed with glioblastoma experience symptoms like seizures, persistent headaches, or loss of brain function like memory loss and personality changes. Glioblastomas have devastating consequences for patients. The median survival time is 12 to 14 months, and less than 7% of patients survive more than five years. Thus, better treatments and strategies for improving prognosis are urgently needed as there is no cure for the disease.
Researchers analyzed the blood samples of 441 glioblastoma male and female patients to evaluate the correlation between the TSPO polymorphic variant rs6971, one of the most frequent polymorphisms (variants) found in humans, with the clinical outcomes of glioblastoma patients. Compared with female glioblastoma patients, males with the TSPO variant had shorter overall and progression-free survival times. There was no association between the variant and survival time in females. The study suggests that as a predictor of poor prognosis, the variant has potential for use as a prognostic biomarker in glioblastoma patients.
“We have been thinking about sex differences in glioblastoma in terms of immune responses and this collaborative study provides an unexpected example of a polymorphism that shows a sex difference, suggesting that there are likely others that function in a similar manner,” said Justin D. Lathia, vice chair of the Department of Cardiovascular & Metabolic Sciences at Cleveland Clinic’s Lerner Research Institute and one of the study’s senior authors. “This is an exciting new direction and will be the focus of future studies.”
The research team also included colleagues from the National Cancer Institute led by Jill Barnholtz-Sloan, associate director, informatics and data science, in the Center for Biomedical Informatics and Information Technology and senior investigator in the Division of Cancer Epidemiology and Genetics.
Azzam said this will be the first of many studies related to the use of TSPO as a prognostic biomarker.
“What we really need to do is understand the function of this polymorphism. Why is it associated with worse survival in male patients? Why do we see biological sex-specific differences? We have so many questions now,” she said.
Stephanie Rendon, Florida International University

