A dosing error made during an AstraZeneca-University of Oxford COVID-19 vaccine trial has led to a new dosage finding in mice, reports a new Northwestern Medicine study.
During the AstraZeneca-Oxford trial, some human participants erroneously received a half dose of their first shot, followed by a full dose for their second shot. Paradoxically, the trial showed that volunteers who got a lower dose of the first shot were better protected against COVID-19 than those who received two full doses.
However, it was not clear if the improvement of the low-dose vaccine was due to the dose itself or the fact that people who received the lower dose had also had a longer time between the first and the second shot, known as an extended prime-boost interval.
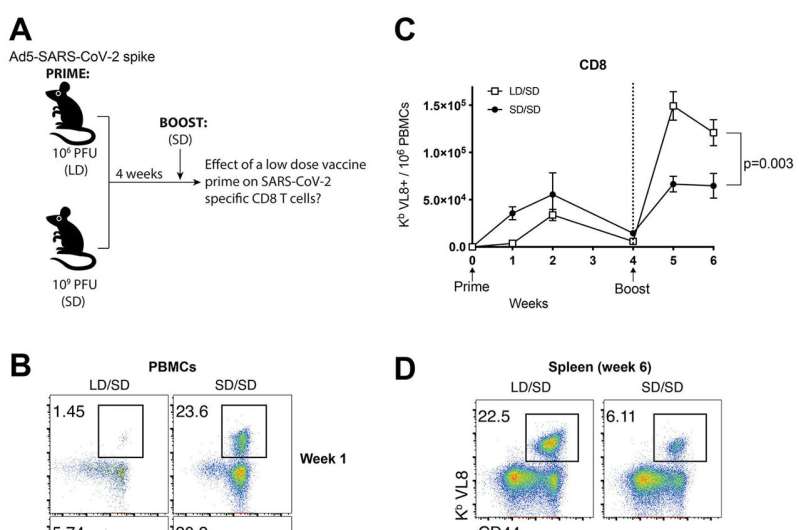
Scientists from Northwestern University Feinberg School of Medicine tested the effect of a SARS-CoV-2 vaccine prime dose in mice and found that a lower-dose first shot, followed by a full-dose booster shot, significantly improved the potency of a SARS-CoV-2 vaccine. The booster shot produced more antibodies and T-cells in the mice, allowing them to develop much more robust immune responses against SARS-CoV-2, the study found.
The findings were recently published in the journal Science Immunology.
Study questions idea of ‘dose escalation’ in vaccine trials
Vaccine clinical trials use a method known as dose escalation, in which one person receives a lower dose and is boosted with that same lower dose; a second person receives a higher dose and is boosted with that same higher dose, and so on.
“The idea is to make sure the vaccine is safe, so scientists use dose escalation to determine the ‘goldilocks zone’: what is the minimum dose of vaccine that you can give to someone while still getting a good immune response?” said lead author Pablo Penaloza-MacMaster, assistant professor of microbiology-immunology at Feinberg.
The Northwestern study did not use the AstraZeneca-Oxford vaccine but instead used one that was similar: an adenovirus serotype 5 vaccine that is akin to the Chinese-developed CanSino and Russian-developed Sputnik V vaccines. Penaloza-MacMaster said their ongoing studies are now examining this dosing regimen in mRNA vaccines.
Why did the lower dose/standard dose work better?
In the AstraZeneca trial, participants who received the full first dose were boosted around three to four weeks after the first shot whereas those who received the lower dose had a much more extended prime-boost interval. The Northwestern study replicated this extended prime-boost interval in mice, and also reported that increasing the prime-boost interval improves the immune response.
“An extended prime-boost interval allows the immune system to rest and mature in a way that the immune response can then expand more robustly upon a booster vaccination,” Penaloza-MacMaster said. “The longer you wait before boosting, the better that secondary immune response will be.”
This can be a tricky game, though, he said, because waiting longer to boost might increase one’s susceptibility of getting the virus.
“With a pandemic, it’s ethically challenging to extend that prime-boost interval because you need people to get fully protected as soon as possible,” Penaloza-MacMaster said. “But this approach may have its benefits in terms of improving the durability and magnitude of immune responses in the long run, which may be useful not just for SARS-CoV-2 vaccines, but also for other vaccines.”
The team also observed similar positive effects of lowering vaccine doses with an experimental HIV vaccine based on an adenovirus vector, suggesting that these findings may be generalizable to other vaccines.
Kristin Samuelson, Northwestern University

