Writing in EMBO reports, researchers at University of California San Diego School of Medicine and Moores Cancer Center at UC San Diego Health describe how a pair of fundamental genetic and cellular processes are exploited by cancer cells to promote tumor survival and growth.
The findings appear in the October 26, 2021 issue of the journal, a publication of the European Molecular Biology Organization.
Cancer is driven by multiple types of genetic alterations, including DNA mutations and copy number alterations ranging in scale from small insertions and deletions to whole genome duplication events.
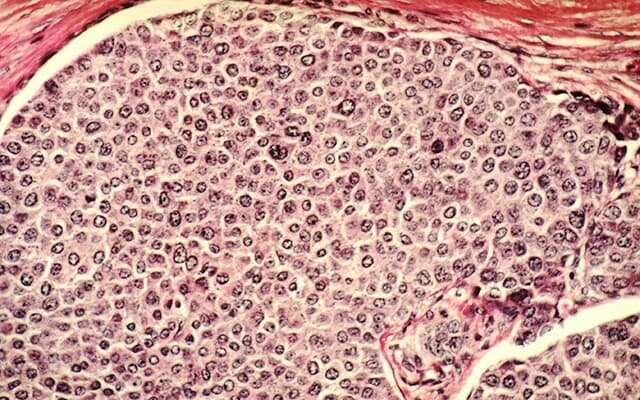
Collectively, somatic copy number alterations in tumors frequently result in an abnormal number of chromosomes, termed aneuploidy, which has been shown to promote tumor development by increasing genetic diversity, instability and evolution. Approximately 90 percent of solid tumors and half of blood cancers present some form of aneuploidy, which is associated with tumor progression and poor prognoses.
In recent years, it has become apparent that cells cohabiting within a tumor microenvironment are subject not only to external stressors (mainly of metabolic origin, such as lack of nutrients), but also to the internal stressor aneuploidy. Both activate a stress response mechanism called the unfolded protein response (UPR), which leads to an accumulation of misfolded proteins in the endoplasmic reticulum (ER) of cells—an organelle that synthesizes proteins and transports them outside the cell.
When this primary transport/export system is disrupted, UPR attempts to restore normal function by halting the accumulation of misfolded proteins, degrading and removing them and activating signaling pathways to promote proper protein folding.
If homeostasis or equilibrium is not re-established quickly, non-tumor cells undergo cell death. Conversely, cancer cells thrive in this chaos, establishing a higher tolerance threshold that favors their survival.
“In these circumstances, they also co-opt neighboring cells in a spiral of deceit that progressively impairs local immune cells,” said co-senior author Maurizio Zanetti, MD, professor of medicine at UC San Diego School of Medicine and a tumor immunologist at Moores Cancer Center with Hannah Carter, Ph.D., associate professor of medicine and a computational biologist. Zanetti had previously introduced the hypothesis in a Science commentary.
The researchers hypothesized that aneuploidy, UPR and immune cell dysregulation could be linked together in a deadly triangle. In the new study, Zanetti, Carter and colleagues analyzed 9,375 human tumor samples and found that cancer cell aneuploidy intersects preferentially with certain branches of the signaling response to stress and that this finding correlates with the damaging effects of aneuploidy on T lymphocytes, a type of immune cell.
“This was an ambitious goal not attempted before,” said Zanetti. “It was like interrogating three chief systems together—chromosomal abnormalities in toto, signaling mechanisms in response to endogenous stress and dysregulation of neighboring immune cells—just to prove a bold hypothesis.”
“We knew the task would be challenging,” added Carter, “and that we would need to create and refine new analytical tools to test our hypotheses in heterogeneous human tumor data, but it was a worthwhile risk to take.”
The findings, they said, show that the stress response in cancer cells serves as an unpredicted link between aneuploidy and immune cells to “diminish immune competence and anti-tumor effects.” It also demonstrates that molecules released by aneuploid cells affect another type of immune cells—macrophages—by subverting their normal function to turn them into tumor-promoting actors.
The findings offer new opportunities to understand tumor progression as a balance between the progressive accumulation of chromosomal abnormalities during tumor evolution and the progressive decay of anti-tumor immunity, said the authors, with the signaling response to stress gauging and regulating the relationship.
In practical terms, they said, a new aneuploidy score defining the burden of chromosomal abnormalities, developed for the study, could set a new paradigm for assessing the biological stage of tumor progression in patients and be used to extrapolate immune status.
“It may also inform on new opportunities for pharmacological or genetic interventions that interfere with specific branches of the UPR as the mediator of aneuploidy-driven local immune dysregulation. This non-immunological approach could make immunotherapy of cancer more efficient,” said Zanetti.
Co-authors include: Su Xian, Magalie Dosset, Gonzalo Almanza, Stephen Searles, Paras Sahani, T. Cameron Waller, Kristen Jepsen and Hannah Carter, all at UC San Diego.
Scott Lafee, University of California – San Diego

