Each year, about half a million children in Africa die from malaria. Infection with the malaria parasite is such a widespread and deadly disease that scientists all over the globe are working to understand it better in order to be able to fight it.
Now, researchers from the University of Copenhagen have come a significant step closer, as they have found an important difference between naturally acquired immunity and immunity following vaccination.
“The antibodies which the body produces when you have been infected with malaria look different from those produced by the body when you have been vaccinated. And that probably means that our immune system has a more efficient response when we have been naturally infected than when we are vaccinated against malaria,” says Lars Hviid, Professor at the Department of Immunology and Microbiology.
‘Natural killer cells’
The immune system can trigger various mechanisms in order to defend the body. The usual defense against infections with parasites, viruses and bacteria consists of so-called macrophages.
“When we are exposed to an attack from the outside, the immune system can produce antibodies that attach to the foreign body that needs to be fought. They are then recognized by some small cells called macrophages, which are attracted to the antibody and eat the bacterium or virus. This is basically how immunity to most infectious diseases works,” explains Lars Hviid.
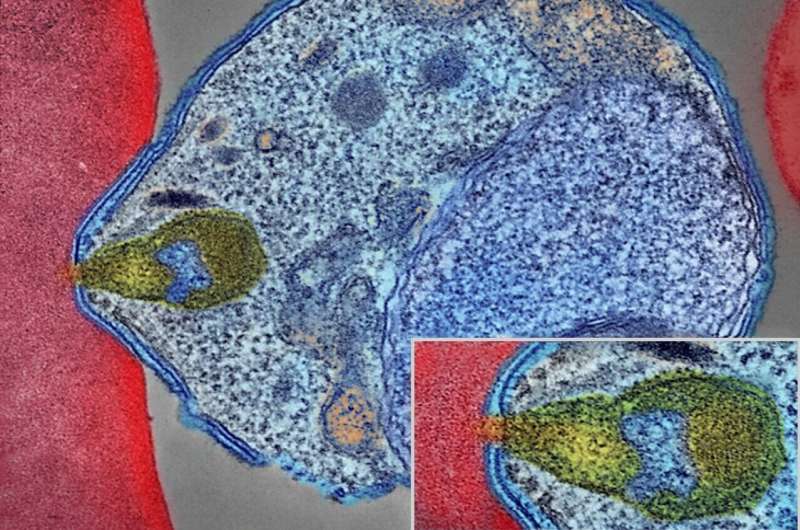
But, now, researchers have discovered that immunity to malaria seems to work differently. Here, the body’s immune system uses some other types of cells to fight an infection with the malaria parasite.
“We have found that the antibodies look different, depending on whether you have been vaccinated or infected. And that means that the body launches some other defense mechanism, as instead, it uses what we call natural killer cells,” says Lars Hviid.
More in common with cancer
Natural killer cells are usually known to researchers as one of the body’s best weapons to fight cancer cells. But, now, it seems that the defense against malaria has features in common with the immune system against cancer.
“In popular terms, you could say that the immune system has a more tailored defense against malaria than against other typical infections. Maybe we have evolved in this way because it is such a contagious and deadly disease—that is difficult to guess,” says Lars Hviid.
The researchers made the findings by comparing blood samples from Ghanaian people who had been infected with malaria with blood samples from people who participated in Phase 1 clinical trials of an experimental malaria vaccine.
He explains that the new knowledge may be used to develop new and improved malaria vaccines.
“Our study points to a new strategy for developing even better malaria vaccines in the future. Because, now, we know how the body mobilizes the defense with natural killer cells, and we can imitate that with vaccines,” he says.
He looks forward to being able to test—together with other researchers—whether a future malaria vaccine will be able to utilize natural killer cells instead of the macrophages that the current vaccines use.
University of Copenhagen

