A study led by researchers at Children’s Hospital of Philadelphia (CHOP) has implicated several genes involved in a variety of bodily functions associated with the hypothalamus, a notoriously difficult-to-study region of the brain. The findings could help clinicians identify potential causes of dysfunction for many important traits regulated by the hypothalamus, such as sleep, stress, and reproduction.
The findings were published today in the journal Nature Communications.
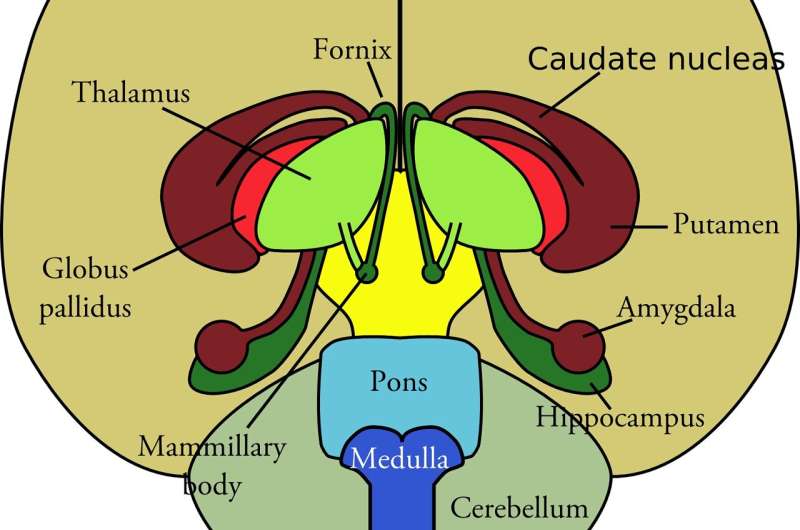
The hypothalamus helps maintain health and stable metabolism by influencing a variety of vital functions, including appetite and thirst, puberty and reproductive timing, sleep cycles, and body temperature. However, the hypothalamus is located in the center of the brain, making it extremely difficult to study the gene regulation associated with these traits.
To overcome that hurdle, the researchers used an embryonic stem cell (ESC) model to study gene expression during development of the hypothalamus. This model allowed them to study the genetic architecture first in hypothalamic progenitor cells—cells prior to their full development into a hypothalamus—and then in arcuate nucleus-like hypothalamic neurons. The hypothalamus contains several different subtypes of neurons, and the researchers integrated results from various genome-wide association studies (GWAS) to implicate genes driving particular traits regulated by the hypothalamus.
“By studying the three-dimensional genomic architecture of these cell models, we can see the dynamic process of how the hypothalamus is formed over different stages of development,” said senior study author Struan F.A. Grant, Ph.D., Director of the Center for Spatial and Functional Genomics and the Daniel B. Burke Endowed Chair for Diabetes Research at CHOP. “The information we yielded in this study provides us with more concrete information about diseases that are relevant to hypothalamic function.”
Grant and his collaborators assessed variants associated with puberty, body mass index, height, bipolar disorder, sleep, and major depressive disorder, among others. They identified both known and novel genes associated with these traits. For example, their data confirmed the role of the BDNF of gene in influencing body mass index and obesity risk. Another gene of interest identified in the study was PER2, which was implicated in sleep regulation.
All the data ascertained from this study will be made publicly available. Many of the disorders studied can be caused by other factors, so the findings will help researchers distinguish which genes play a more central role in this tissue and in turn inform clinical practice. For example, body mass index can be affected by variants in genes conferring their effects in hypothalamus or fat tissue cells, so being able to distinguish the context in which genes and subsequent tissues or hormones operate can lead to more personalized treatment options.
“The data set we derived from this study allows other researchers to determine which diseases or conditions are relevant when doing a genetic workup of the patient,” Grant said. “As more information about the hypothalamus is known, that information can be queried against this data set and potentially identify therapeutic targets for multiple disorders.”
Children’s Hospital of Philadelphia

