Chronic wounds are deep and difficult to repair. Often, the top of the injury heals before the bottom, so the wound collapses in on itself. Over time, this can result in scar tissue and reduced skin function.
In APL Bioengineering, researchers from the University of Birmingham and University of Huddersfield developed an approach to print skin equivalents. The material may play a future role in facilitating the healing of chronic wounds.
The technique is the first of its kind to simulate three layers of skin: the hypodermis, or fatty layer, the dermis, and the epidermis.
“You effectively have three different cell types. They all grow at different speeds,” said author Alan Smith. “If you try to produce tri-layered structures, it can be very difficult to provide each of the requirements of each different layer.”
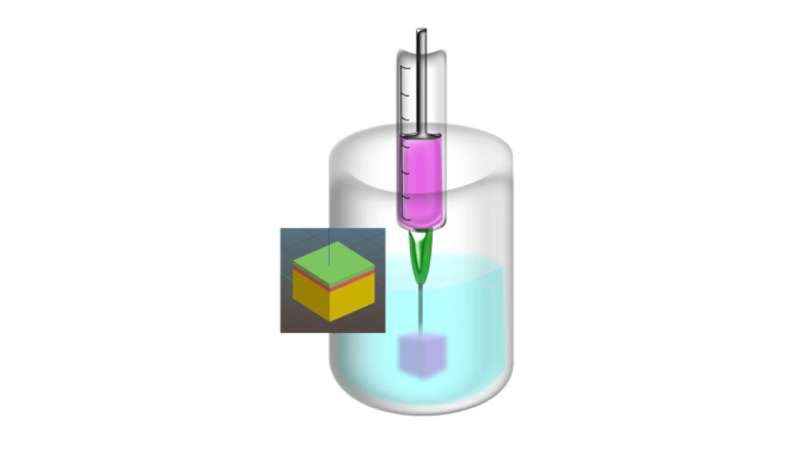
To solve this problem, the scientists used suspended layer additive manufacturing (SLAM). They created a gel-like material to support the skin equivalent, twisting and altering the structure of the gel as it formed to create a bed of particles that can then support a second phase of gel injection.
During printing, the skin layers are deposited within the support gel, which holds everything in place. After printing, the team washed away the support material, leaving behind the layered skin equivalent.
If the researchers moved a needle through the supporting gel, it repaired itself faster than other similar techniques. This results in higher resolution printing than previous methods and allows for the printing of complicated skin structures.
The authors tested the skin substitute by cutting a hole in pig tissue and printing a skin equivalent to fill the hole. After culturing the model system for 14 days, they saw signs of wound repair.
“We used a stain that allowed us to quantify the integration we got between original material and tissue,” said author Liam Grover. “We were able to demonstrate some integration even after a short period of time.”
The team cannot assess chronic wound healing with the skin substitute because that process takes more time than their model allowed, which was only 14-21 days. However, their next step is to test longer, appropriate models for chronic deep wounds. The ultimate goal is to repair human skin and reduce scarring for all patient scenarios.
American Institute of Physics

