Fear of needles is, for part of the population, the main reason for not getting a COVID-19 vaccine. That fear is demonstrated by the fact that needleless techniques have been in development for more than 150 years. A new technology, developed by David Fernandez Rivas and his team, is safer than previous ones, and it is better at steering the injection fluid and controlling the depth to which it penetrates the body. This is reason enough for researcher Jelle Schoppink to compare the different options, in a ‘perspective paper’ in Advanced Drug Delivery Reviews.
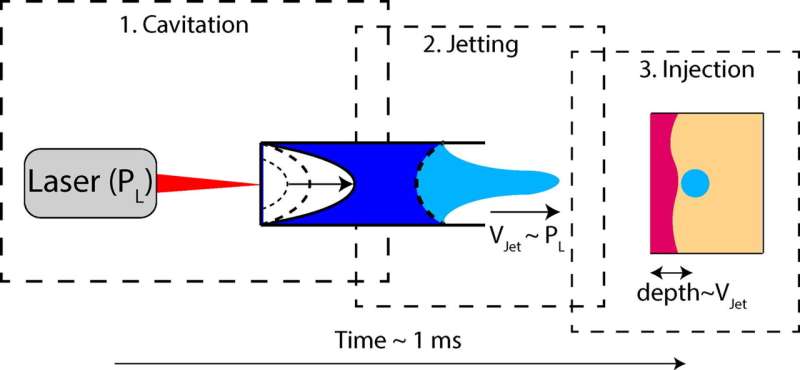
Needle-free injection that uses a liquid jet that is heated and ‘shot’ by a laser is a development that the University of Twente, as well as its spinoff company FlowBeams is working hard on. It takes away barriers for people that are afraid of needles and reduces the huge amount of waste in hospitals. An important property is that the jet can be controlled to a large extent: no more fluid is used than is actually needed, and the dosage depth that is sent to the dermis and epidermis—close to the outer skin surface—is highly controllable.
Cross contamination
The new method is is entirely different from early mass vaccination techniques that were used in the 1950s. In early techniques, the fluid got its speed by the energy stored in a spring that was released. The penetration depth was 2 to 10 millimeter and it was not easy to control. The World Health Organisation (WHO) decided to end this type of vaccination when it was discovered that blood appeared to come back into the injector, with large-scale cross contamination as a result.
Low depth
For about ten years now, the application of lasers seems to be most attractive, after experiments had been done using compressed gas or using piezoelectric devices to generate the necessary force to ‘shoot’ the liquid. Laser powered fluid jets had been developed by the Physics of Fluids group of Professor Detlef Lohse, using a so-called pulsed laser. This is similar to the technology David Fernandez Rivas and his team are currently developing, but they use a continuous laser instead, which has advantages including size and cost. The fluid dynamic is highly controllable, with a typical depth of 0.1 millimeter to 1 millimeter. This is much more precise than the old spring-powered technique. You might expect that the function of the injection fluid might change by heating it, but there are no indications that it does, so far.
The danger of returning jets, can be prevented as well. Although the laser-induced injection technique has not been tested on humans yet, tests on gels that look like human skin and tests on pig skin, show promising results. Replacing a needle clearly is not necessary, but there is a plastic nozzle that has to be replaced for each patient. But according to Schoppink, this will not be necessary in the future, which will reduce the amount of waste even more.
Schoppink also compared the needleless technology to a technique that does use needles, but very tiny, microsized ones that you hardly feel—just like sandpaper. Although these are made using silicon technology and there is an issue with recyclability, these patches of microneedles could be used in combination with the fluidic solution, as a sort of signpost directing multiple jets in the right way.
Schoppink’s article illustrates the advantages of current technology, but also places it in perspective and explores ways of combining techniques for the best patient-friendly solution.
University of Twente

