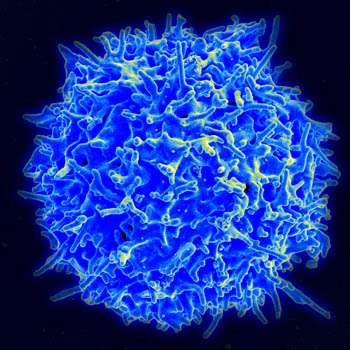
Researchers at University Hospitals Seidman Cancer Center and Case Western Reserve University have developed a novel approach to chimeric antigen receptor (CAR) T-cell therapy for B-cell cancers that triples the targeted antigens on cancer cells—a “back up” approach that promises to greatly reduce the potential for antigen escape currently found in CAR T therapies that solely target CD19.
“Cancer cells are tricky,” says Reshmi Parameswaran, Ph.D., senior author of a new paper in the journal Nature Communications outlining the new approach and a scientist in the Division of Hematology and Oncology at UH Seidman Cancer Center. “The cancer cells will shed the CD19 antigen and suddenly become CD19-negative and therefore not respond to the CD19 CAR T therapy. Thus, there is a great need to identify alternative targeting strategies and CAR designs. With the BAFF CAR T, we hope that even if one receptor is lost, the others will do the job. Also, cancer cells that do not express CD19 but express BAFF receptors can be targeted, such as multiple myeloma.”
The new B-cell activating factor (BAFF) CAR T product developed here binds specifically to each of three receptors instead of one—BAFF-R, BCMA and TACI, providing more therapeutic options. At least two of these three receptors are found in almost all B cell cancers, with some cancers expressing all three. Experimental results reported in Nature Communications show that the BAFF CAR T is effective at killing multiple B-cell cancers.
“We show that these BAFF CART-cells are both functional and specific in targeting the three BAFF receptors (BAFF-R, BCMA and TACI) expressed by multiple B-cell cancers,” Dr. Parameswaran says. “We demonstrate robust in vitro and in vivo cytotoxicity exerted by BAFF CAR T-cells against mantle cell lymphoma, multiple myeloma and acute lymphoblastic leukemia xenograft mouse models.”
An Investigational New Drug (IND) application to the U.S. Food and Drug Administration will be filed in the coming weeks with partner Luminary Therapeutics and the team looks to launch a clinical trial of BAFF CAR T therapy in patients with non-Hodgkin lymphoma in the next several months. The work of expanding BAFF CAR T-cells is well under way. It is being done on site at the Cellular Therapy Lab jointly operated by the Wesley Center for Immunotherapy at UH Seidman Cancer Center and the National Center for Regenerative Medicine at Case Western Reserve University. This state-of-the-art cell manufacturing facility is capable of generating CAR T-cells in an expedited fashion and at reduced cost.
Dr. Parameswaran, also an Assistant Professor of Medicine at Case Western Reserve University School of Medicine, has been working on BAFF applications since 2008 and has long thought a BAFF ligand protein had potential as a CAR T vehicle. She credits Stan Gerson, MD, Acting Director of the Case Comprehensive Cancer Center and Dean of the Case Western Reserve University School of Medicine, with encouraging her team’s work. “Always when he saw me, he would ask, “What’s going on with your BAFF CAR T? Please do it, Reshmi, it’s important,'” she says. “Those words gave me encouragement. Case Comprehensive Cancer Center gave me some pilot money at that time to do the project. Luckily, when we tried, it worked.”
Because the new BAFF CAR T is based on a ligand protein and not merely an individual antibody fragment, it can target all the BAFF receptors on the cancer cell.
“That’s the beauty of it—it’s a ligand-based CAR and can target three receptors, so it’s not just single targeting,” Dr. Parameswaran says.
The BAFF CAR T also has other clear advantages, she says. Unlike CAR T products that target CD19, which kill both early and mature B cells, the BAFF CAR T spares early B cells because these cells do not express BAFF receptors.”In patients receiving CD19 CAR T therapy, there is B cell aplasia, so B cells are depleted,” she says. “Using the BAFF CAR, the early B cells will not be killed, and it’s easy for the early B cells to replenish the mature cells. We are not really anticipating the B cell aplasia seen in CD19 therapies.”
Because of this early success, Dr. Parameswaran says, Case Western Reserve University has signed an exclusive option agreement with pharmaceutical company Luminary Therapeutics for the technology, which includes an option for Luminary to exclusively license a novel BAFF target for use in CAR T constructs. Luminary Therapeutics has special expertise in the non-viral transposon method of delivering BAFF CAR T-cells outlined in the Nature Communications paper.
“Currently, the production of CAR-Ts is primarily achieved using viral transduction of transgenes into primary human T cells,” she says. “However, since the first human application of transposon-mediated gene therapy almost 10 years ago, a dozen more clinical trials are under way or have been completed, supporting transposon-based systems as a safe and stable gene transfer alternative with comparable or superior efficiencies to viral transduction.”
Dr. Parameswaran says she hopes her team’s success with the new BAFF CAR T will lead others to pursue other novel approaches to the quickly emerging therapy. “Of the CAR-T cell therapies in clinical development, a third still target CD19, the same target as the currently approved CD19 CAR T therapies,” she notes. “Beyond CD19, 70% of these clinically investigated CAR T therapies are directed against just 10 antigens, reflecting a significant duplication of targets.”
She says she’s also encouraged by what this new research could mean for patients, even in the very short term, in terms of reduced side effects from CAR T therapy. “CD19 CAR T-cell therapy adverse effects include severe B cell aplasia, due to pan-B-cell expression of the CD19 marker,” she observes. “Unlike CD19 CAR T-cells, BAFF CAR T-cells designed to target BAFF receptors may produce less severe B-cell aplasia, as the BAFF receptors are not expressed by early-stage B-cells. Unaffected early B-cells could easily replenish the mature B-cell population.”
University Hospitals Cleveland Medical Center

