Older stroke patients who had a history of COVID-19 were more likely to develop dangerous blood clots in the veins than those who did not have the coronavirus-driven disease, a new study from the Centers for Disease Control and Prevention shows.
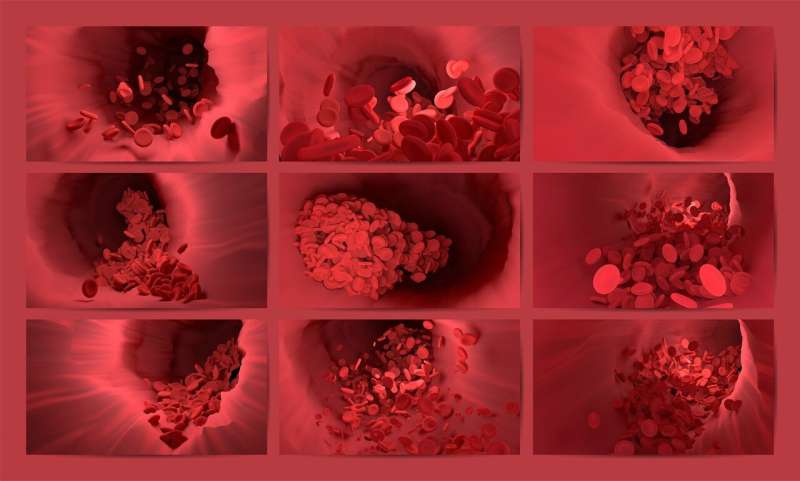
Blood clots that form in veins, a condition called venous thromboembolism or VTE, are a common complication after stroke. Clots can form in a leg or elsewhere, then may break free and block blood supply to the lungs, causing often fatal pulmonary embolism.
Several studies suggest SARS-CoV-2, the virus that causes COVID-19, may increase the risk of VTE among people hospitalized with COVID-19, said Xin Tong, the new study’s senior researcher and a senior statistician in the CDC’s Division of Heart Disease and Stroke Prevention.
But Tong said few studies examined the association between COVID-19 and VTE risk among people with an acute ischemic stroke, the most common type of stroke in which a clot in an artery blocks blood flow to the brain. And none had examined this association between VTE and stroke patients who’d had mild symptoms of COVID-19 that did not require hospitalization.
Tong and her co-authors used Medicare data to examine the association between VTE and COVID-19 among 235,567 Medicare beneficiaries ages 65 and older. All had been hospitalized with an acute ischemic stroke between April 2020 and November 2021.
Among them, 7.8 percent had a history of COVID-19, which required hospitalization for slightly more than half.
VTE was most common among those with a history of COVID-19 hospitalization, at 4.4 percent. Among those with COVID-19 that had not required hospitalization, 3.1 percent had VTE. Those without a history of COVID-19 were least likely to have VTE, at 2.6 percent.
That translated to a 64 percent higher risk of VTE among stroke patients with a history of COVID-19 hospitalization, and a 21 percent higher risk among those who’d had COVID-19 but didn’t need to be hospitalized.
The study will be presented next week at the American Stroke Association’s International Stroke Conference. The findings are considered preliminary until a full paper is published in a peer-reviewed journal.
Researchers also found that Black stroke patients had the highest rate of VTE compared to other racial and ethnic groups. For example, 6.3 percent of Black stroke patients who’d previously been hospitalized for COVID-19 had VTE. That compares to 3.4 percent and 4.1 percent of their Hispanic and white counterparts, respectively.
Among the limitations the researchers acknowledged was they could not identify if the VTE happened before or during the stroke hospitalizations.
Despite that, and limits on what can be understood about some racial and ethnic groups because of small numbers of patients, the study provides “a good big-picture overview of what we’re seeing” across the country, said epidemiologist Amelia K. Boehme of Columbia University in New York City.
“We know that COVID increases the risk of VTE,” said Boehme, who was not involved in the research. “We know that ischemic strokes increase the risk of VTE. So the idea that combined COVID and ischemic stroke would further increase the risk of VTE makes sense from a clinical perspective.”
The study suggests that stroke patients who’ve had COVID-19 should be carefully monitored for potential VTE, she said.
The possible reasons behind a link between COVID-19 and an increased risk of VTE are complex and not well understood, Tong said. Some underlying conditions of stroke patients can overlap with VTE risk factors, which include older age, prolonged immobility, obesity, and prior VTE or stroke.
Some of those same factors overlap with risk of severe COVID-19.
“Further studies are needed for the likely mechanisms between COVID-19 and increased risk of VTE,” Tong said. Meanwhile, she said, doctors should be aware of the association and follow protocols for early prevention and treatment.
Michael Merschel, American Heart Association

