What is going on at the single-cell level in the first days of SARS-CoV-2 infection in the lungs?
Researchers at Texas Biomedical Research Institute and Southwest National Primate Research Center (SNPRC), in collaboration with Washington University in St. Louis, have clarified what immune cells are present in the lungs in the first days of SARS-CoV-2 infection, and what some of those cells are doing to fight off the virus. The findings, reported in Nature Communications this week, will help guide the development of future treatments for COVID-19.
“This is the most detailed analysis of early SARS-CoV-2 infection to date thanks to the latest single-cell sequencing technologies, and animal models developed at Texas Biomed and SNPRC,” says Deepak Kaushal, Ph.D., SNPRC Director and senior paper author.
The analysis has shed light on a key mystery throughout the COVID-19 pandemic: The role of a class of signaling proteins called Type I Interferons (IFN). During viral infections, interferon molecules act like sentries or alarm bells, blaring “Intruder alert!” to other cells, so they can boost their defense systems. However, some reports have shown a lower Type I Interferon response to SARS-CoV-2, allowing the virus to spread more readily. At the same time, runaway interferon “cytokine storms” have been a hallmark of severe COVID-19.
Scientists have been trying to figure out if interferon fights SARS-CoV-2 or is somehow dysregulated, especially early on in infection. Clarifying this is important for developing treatments that aim to limit harmful inflammation linked to excessive interferon activity, without blocking its protective mechanisms.
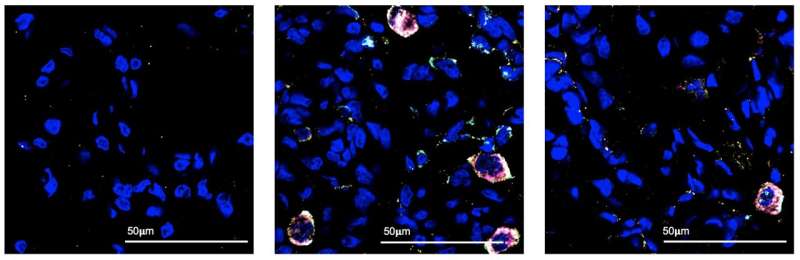
This new research shows interferon plays a key role in clearing the virus, by alerting other immune cells, called macrophages, to search and destroy the virus. Macrophages are akin to Pac-Man, gobbling up cells infected with the virus.
“Our analysis shows there is a massive population of macrophages in the lungs at day three after infection, amounting to 80 to 90 percent of all cells in the airways at that moment,” says Dhiraj K. Singh, Ph.D., a staff scientist at Texas Biomed and first paper author. “We can also tell by looking at the genes that are activated in those macrophages, that they are specifically responding to an interferon signal.”
The finding was possible thanks to the latest, highest-resolution genetic sequencing technology: Single-cell RNA sequencing. The team sequenced the gene expression profiles of more than 170,000 individual cells. These profiles, which tell them which genes are turned up or down, indicate what the cell is and what it is doing at the time. Singh worked closely with Shabaana Khader, Ph.D., and Maxim Artyomov, Ph.D., and their teams at Washington University in St. Louis to analyze and interpret the massive amounts of raw, high-resolution data.
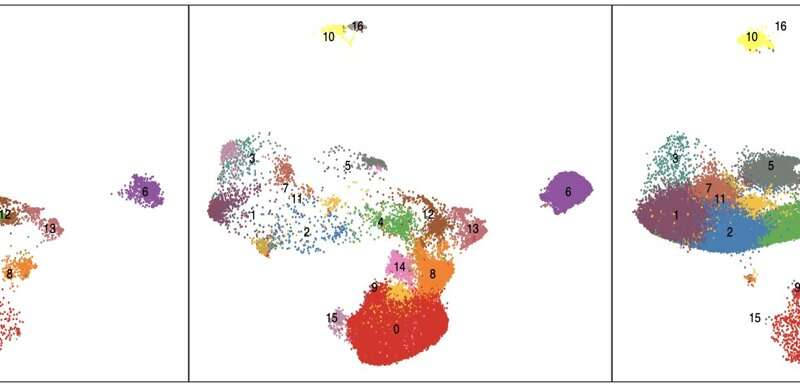
“RNA sequencing has been around for 10 years, but it averages out gene expression activity for an entire tissue,” Singh says. “In contrast, the latest single-cell RNA sequencing can tell you what genes are on and off in say, B cells versus T cells. It is so much more specific.”
But the data could not have been collected in the first place without animal models. To get a snapshot of the lung environment before, during and after infection, scientists collect what amounts to a lung wash at key time points from rhesus macaques.
“Often, by the time people go to the clinic when they are sick, the virus is already well established,” Singh says. “Primates are the only model where we can actually look at those early acute responses.”
Kaushal underscored how at the start of the COVID-19 pandemic, the San Antonio community rallied behind Texas Biomed and SNPRC, donating more than $5 million in a week to support the institute’s efforts to develop animal models for COVID-19 research. The animal models have since been critical for testing vaccines and therapies, including the Pfizer-BioNTech vaccine and Regeneron’s monoclonal antibody cocktail.
“This new research is a continuation of the animal model that we generated, which would not have been possible without the generous contribution of the San Antonio community and ongoing support from the National Institutes of Health’s Office of Research Infrastructure Programs,” Kaushal says. “It shows once you’ve established a model, what is possible. You can really advance knowledge in the area.”
Singh has recently received a San Antonio Medical Foundation grant to see what happens when more interferon is added to the lungs, and compare that with other ongoing studies blocking interferon. If the studies ultimately confirm interferon’s positive role in marshaling macrophages early in infection, it could potentially lead to interferon-based therapies for COVID-19. These have been tried for other diseases, and so could move quickly to clinical trials.
“In my opinion, the potential applications don’t stop at COVID-19,” Kaushal says. “It’s quite likely that the next pandemic in the next 10 years or so will be caused by another coronavirus. So having all this knowledge is going to be very critical.”
Texas Biomedical Research Institute

