Glioblastoma is an aggressive cancer that can occur in the brain or spinal cord. It can occur at any age, but glioblastoma is more common in older adults. The average age of diagnosis is 64.
Also known as glioblastoma multiforme, glioblastoma can cause worsening headaches, nausea, vomiting and seizures. Symptoms vary based on the tumor’s size, location and rate of growth. Glioblastoma also can cause confusion or decline in brain function, memory loss, difficulty with balance, and vision problems ― symptoms an older person might mistake for the aging process.
“Younger patients tend to be more aware of these small changes, and they go see a doctor if they really notice a change,” says Sujay Vora, M.D., a Mayo Clinic radiation oncologist. “Older patients, if they’re having problems with memory or sharpness of thinking, may think it’s due to other causes and not connect it with a brain tumor. This can cause a delay in diagnosis and treatment.”
Treatments may reduce such symptoms and slow the progression of glioblastoma, but a cure is often not possible. When it comes to developing a care plan, it’s important to weigh the benefits of treatment against side effects that might reduce quality of life. “For older patients, a lot depends on other health issues and their overall physical condition,” says Dr. Vora.
Treating glioblastoma along with other health conditions
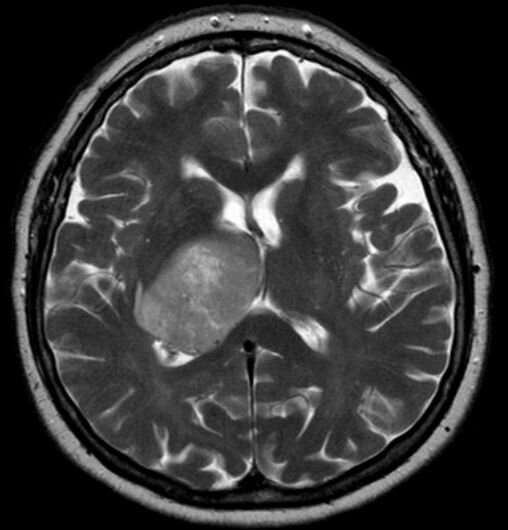
If a brain tumor is suspected based on a neurological exam, a person will typically receive an MRI (Magnetic resonance imaging). This test uses a magnetic field and computer-generated radio waves to create detailed images of organs and tissues.
If an MRI confirms the likelihood of glioblastoma, the next step is a discussion with a neurosurgeon, or brain surgeon. Doctors must consider multiple factors including age, tumor location, nearby brain tissue and a person’s ability to successfully recover from surgery to remove the tumor.
Even if a person is healthy enough to undergo surgery and fully recover, complete removal of the tumor isn’t possible because glioblastoma grows into normal brain tissue. “The surgeon’s job is to not only make the diagnosis, but also to remove as much of the tumor as safely as possible,” says Dr. Vora.
After surgery has been considered or completed, the next phase of glioblastoma treatment is radiation, often paired with oral chemotherapy. For elderly people who have other health conditions or who are unable to care for themselves, multiple trips to receive treatments that may cause unpleasant side effects can be burdensome.
“If a patient is fully able to take care of themselves, and they don’t need any help, that’s a good indicator of how they’ll handle treatment,” says Dr. Vora. “But if they need help, or they’re already somewhat debilitated, we’ll probably offer a shorter course of treatment.”
The standard course of radiation is six weeks. “In older patients, we tend to do shorter courses of radiation ― between one to three weeks,” he says. “In determining the best treatment plan, we need to consider the best interests of the patient.”
“I have a 70-year-old patient without other medical problems who was able to have his entire tumor removed,” says Dr. Vora. “He also had genetics suggesting he would respond favorably to chemoradiation. In such a situation, we may treat the patient with a full six weeks of radiation.”
“I also have a 70-year-old who has cardiac disease and lung disease that limits his mobility, so a shorter radiation treatment schedule makes more sense for him,” he says.
Joe Dangor, Mayo Clinic

