COVID-19 has put a spotlight on the pulmonary and nervous systems, but there is still much to learn about how they interact. Researchers at University of California San Diego School of Medicine recently explored this relationship in the context of a childhood lung disease, but their findings may also apply to COVID-19 symptoms.
In a study published March 17, 2022, in the journal Developmental Cell, scientists show that excessive neuropeptide secretion by neuroendocrine cells in the lungs can lead to fluid buildup and poor oxygenation; blocking the neuropeptides may be an effective treatment.
Neuroendocrine cell hyperplasia of infancy (NEHI) is a lung disease affecting infants in which lung size and structure appear normal but blood-oxygen levels are consistently low. There is no disease-specific treatment available for NEHI, and most children require supplemental oxygen for many years.
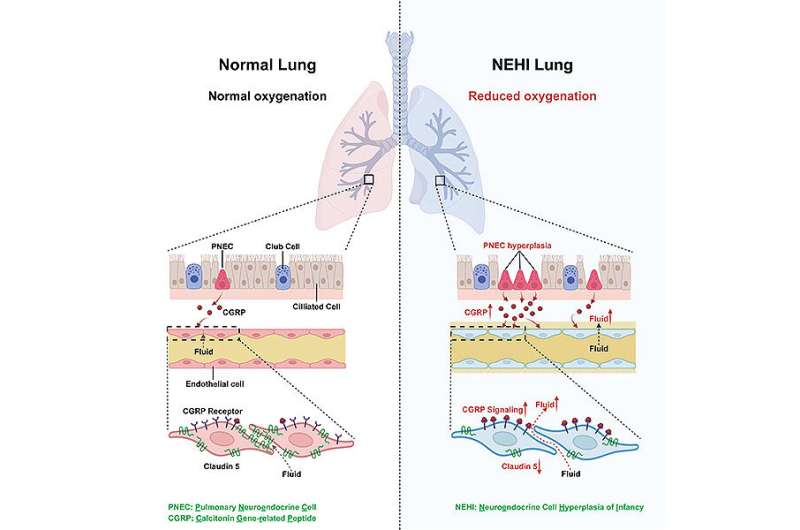
The defining feature of NEHI is an increase in the number of pulmonary neuroendocrine cells (PNECs), a type of lung cell with many neuronal properties. These cells serve as a gateway between the nervous system and the lung, taking in signals about the air environment and directing the lung to respond. But until now, physicians did not know how these cells contribute to the disease, or if they merely proliferate in response.
In the new study, a team led by senior author Xin Sun, Ph.D., professor of pediatrics at UC San Diego School of Medicine and the Division of Biological Sciences, confirmed that a developmental increase in PNECs is what drives NEHI, and revealed how these neuron-like cells can disrupt lung function.
Using the first genetically engineered mouse model of NEHI, Sun’s team found that the overabundance of PNECs leads to excess secretion of their neuropeptide products. This includes calcitonin gene-related peptide (CGRP), a potent vasodilator.
In healthy lungs, oxygen and carbon dioxide move between the lung epithelium and the blood vessel endothelium in a process known as gas exchange. In NEHI, increased CGRP signals trigger a molecular sequence that weakens the seal between endothelial cells, making the blood vessels more permeable. This allows fluid to leak out of the blood vessels and into the lung, covering cells under a layer of liquid. Gasses then have to pass through this additional fluid layer, which disrupts the gas exchange process and lowers blood oxygenation.
“We were surprised to find that neuropeptides can play such a major role in gas exchange,” said Sun. “Researchers are just starting to appreciate the relationship between the nervous system and the lungs, but the more we understand it, the more we can modulate it to treat disease.”
First author Jinhao Xu, a Ph.D. student in the UC San Diego Division of Biological Sciences, showed that blocking CGRP signals with receptor antagonists could protect the endothelial barrier and improve oxygenation in NEHI mice. These findings suggest that neuropeptides may be a promising therapeutic target for conditions marked by excess lung fluid.
One such condition is acute respiratory distress syndrome (ARDS), a lung condition with multiple causes, including SARS-CoV-2 infection. In patients with COVID-19-associated ARDS, excess fluid is the primary cause of death.
Through collaborations with other UC San Diego School of Medicine faculty, the researchers were able to obtain lung tissue samples from COVID-19 patients. They found the samples also had an increased proportion of CGRP-secreting PNECs, suggesting the same mechanism may contribute to the excess fluid in COVID-19 lungs.
Sun notes that several CGRP and CGRP-receptor antagonists have already been approved by the U.S. Food and Drug Administration for the treatment of migraines, so future clinical trials could evaluate their potential to improve lung function.
“This study was a community effort between many researchers and physicians at UC San Diego,” said Sun. “Through these collaborations, we were able to take our work from the bedside to the bench. Our next steps are to help close this loop and bring our findings back to the patients.”
Nicole Mlynaryk, University of California – San Diego

